Oncology Xenograft Models: Using mice to test cancer treatments
My posting schedule has been sporadic of late because work has gotten in the way. However, the big developments going on in the SteemSTEM community have finally spurred me to start contributing more regularly. This contribution is on a little-known technique that plays a major role in curing cancer.
The cure for cancer has been one of the most elusive goals of modern medical science. This partly because there are many many many different types of cancer, and each type requires a specific treatment. Even when a cancer is identified, researchers will still have to test any potential treatments before they can be applied in a medical setting. In this article, I want to discuss one such tool that has given scientists a lot of help in testing cancer treatments: Xenograft Models.
What is it?
An oncology xenograft model usually refers to a mouse that can grow human cancer cells 1. Often these mice are immunocompromised so their immune system won’t attack the foreign cells 2. Tumor cells are injected into these mouse models and given several weeks to grow. Once the tumor is actively growing, scientists can test different treatments on the cancer to see what is and isn’t effective.

An immunocompromised mouse is injected with cancerous cells and a tumor forms after several weeks 1.
The strain of mouse used in this experiment can have a big impact on the results. Originally, researchers used strains without functioning immune systems 3. This gave the greatest chance for the tumor cells to grow, but the immunocompromised environment they grew in wasn’t very realistic compared to a human body. The development of humanized mice provided a potential solution to this problem. Humanized mice are genetically engineered to be born with a non-functional immune system, but they can be injected with human bone marrow to create an immune system that functions similarly to that of a human 4. This provides a much more realistic environment for tumor cells to grow, but these mice require more work to prepare.

A variety of tumors and cancerous cells lines can be injected into the mouse. In some cases, a doctor can remove a tumor from a human, cut it into tiny pieces and implant a piece into a mouse. This is effective in examining a specific type of cancer, but the cells may not grow depending on the type of cancer and the strain of mouse. To get around this, researchers may use established cell lines 6. For example, if a scientist has a potential treatment for lung cancer, they can find a lung cancer cell line that’s known to grow well in a specific mouse model and use them together.
Why is it important
The main reason researchers use Xenograft models is to save time. These experiments can be done within a few weeks while comparable experiments, like genetically engineering a strain of mice that grows a particular type of cancer, would take orders of magnitude longer by comparison. The several week timespan is fast enough that a patient with a novel type of cancer could conceivably get a viable treatment plan before the cancer spreads too far 7.
The other advantage to xenografts is the cost. A lab can maintain a strain of immunocompromised or humanized mice without too much trouble and grafting cancer onto groups of mice doesn’t require expensive reagents or equipment. Xenografting also bypasses some of the need for additional analytics. A cancerous cell’s genome may not need to be sequenced right away if a xenograft reveals a viable treatment.
Unfortunately, the low time and cost of xenograft mouse models comes at the loss of accuracy and knowledge. Just because a treatment works in this type of oncology model doesn’t mean it will work in a patient. It also doesn’t give researchers much of a clue as to why a treatment works. They’ll still have to do rigorous genetic analysis to determine the genetic mutations that led to the cancer and even further experiments to determine what the treatment is doing to the tumor cells.
Despite these limitations, xenograft models are such an integral part of cancer research that numerous biotech companies sell humanized mice 8 and cancerous cell lines 9. The academic field is flooded with papers that attempt to improve upon our current set of xenograft models and the ways we can use them. The pace of research on this subject doesn’t seem to be slowing down either. To give you an idea of the type of work in this field, I’m going to do a deep dive of a recent paper that uses a xenograft model to validate a potential cancer drug.
Testing a drug that prevents Ewing sarcoma metastasis
The paper “Inhibition of porcupine prolongs metastasis free survival in a mouse xenograft model of Ewing sarcoma” by Hayashi et al. 10 is a great example of why a researcher might want to use xenograft models. Ewing sarcoma is a rare type of cancer that can usually be cured, but has to be treated aggressively because it has a tendency to spread quickly 11. This tendency to spread, also known as metastasis, is what the authors of the paper wanted to focus on. Previous work had identified a drug called WNT974 that inhibits a key pathway leading to metastasis known as Wnt signaling 12, and the authors wanted to see if this drug was effective on Ewin sarcoma.

The first half of this paper involves a bunch of tests that show how the WNT974 drug affects independently growing Ewing sarcoma cell lines. In brief, the researchers showed that this drug inhibits the Wnt pathway and downregulates metastasis related genes. These results were promising, but they don’t guarantee that the drug will have the same effect when the cancer is progressing through an actual host. Thus, the authors turned to xenograft models.
The initial tests with xenograft models were fairly simple. They injected two groups of mice with Ewing sarcoma cell lines and treated one group with the WNT974 drug while keeping the other group as a control. They compared tumor growth and mouse survival between the two groups. The results when using the EWS1 Ewing sarcoma cell line are shown to the right. As you can see, the drug treatment had minimal effect on the growth of the tumor, but mouse survival still dramatically improved. All the control mice died while all the WNT974 drug treated mice survived. These results followed the authors expectations. Since the drug inhibits metastasis, it won’t get rid of the original tumor, but it will prevent the tumor from spreading.
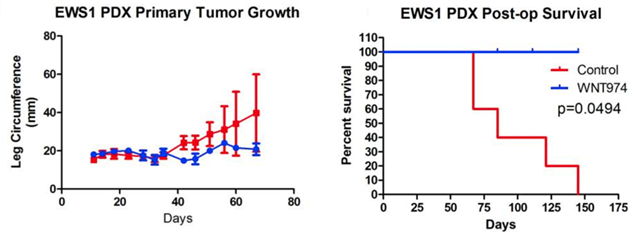
WNT974 increases survival rates, but doesn’t reduce the size of the original tumor (10).
Now that the authors showed that the drug could increase survival rates, they wanted to confirm that it specifically inhibited metastasis in vivo. To do this, they performed a similar experiment in which mice implanted with Ewing sarcoma were treated with and without the WNT974 drug. However, instead of looking at survival rates, they looked at the lungs of all the mice. They were specifically looking for the spread of cancer to the lungs, or in other words, its metastasis. They found that the development of lung metastasis was significantly inhibited when mice were treated with the WNT974 drug.
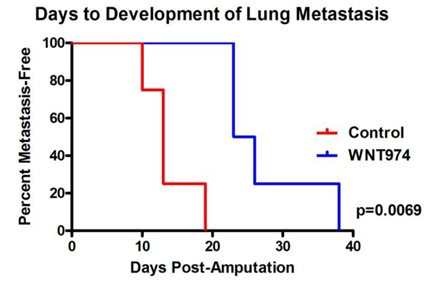
The drug WNT974 delays the onset of lung metastasis in xenograft models (10).
As a final test, the authors injected Ewing sarcoma cell lines directly into the veins of mouse tails. They reasoned that by injecting the cancer cells into the bloodstream, they bypassed the initial steps of metastasis. In this experiment, they found that treatment with the drug WNT974 didn’t have a significant impact on the survival rates of the mice. This suggests that the WNT974 drug inhibits the early steps of metastasis.
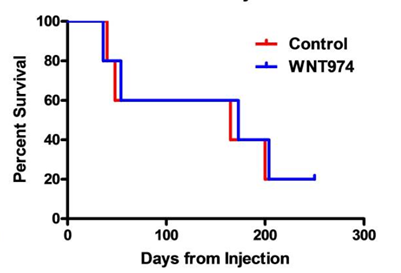
The drug WNT974 doesn’t have an effect when cancer cells are injected directly into the bloodstream (10).
I chose this paper to review because it does a great job of showing how xenograft models can contribute to a good research project. The authors had used a number of preliminary experiments to show that the drug WNT974 was an effective treatment against Ewing sarcoma. However, it was necessary for them to show that this drug was effective in a model that closely resembled cancer progression in a human in a reasonable amount of time. With these criteria, xenograft models were just about the only viable option they could take. This option was nevertheless successful and gave them informative results that rounded out the paper. The authors were also able to show that xenograft models can do more than a simple demonstration of survival rates. Their work showed that the drug specifically inhibited early stages of metastasis.
References
(1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4007037/
(2) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2562196/
(3) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2562196/
(4) https://www.nature.com/articles/nri3311
(5) https://en.wikipedia.org/wiki/Nude_mouse
(6) https://blog.crownbio.com/when-to-use-conventional-cell-line-derived-xenograft-models
(7) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5243815/
(8) https://www.jax.org/jax-mice-and-services/in-vivo-pharmacology/humanized-mice
(9) https://www.crownbio.com/oncology/in-vivo-services/cell-line-derived-cdx-tumor-models
(10) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5667961/
(11) https://en.wikipedia.org/wiki/Ewing%27s_sarcoma
(12) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3864356/
(13) https://pixabay.com/en/porcupines-porcupine-nager-519145/
Images
All images were taken either directly from the publication referenced or labeled for reuse on Google Images. If any image owner has an issue with this article, please contact me and I will address the issue.

This is a very nice review of the article. Although regarding IV of the cell line into the mice - I don't think we can use negative results from this to make a statement about stage at which drug is working. For instance the number of vaiable metastatic cells that may escape from primary tumor into the blood stream may be way less than what IV would deliver. If the number of cells in blood reaching different tisssues is greater than what drug could inhibit, we may see similar results. Now, ofcourse I have not read the paper to know if they did any experiment to rule this out. Though their conclusion would make sense as WNT signalling may work to initiate metastasis, at least from some of talks I have heard. Let me know your views on it.
That’s an excellent point. The authors only say that 10000 cells were injected but don’t mention how much they expect in the bloodstream from typical metastasis. They don’t lean too heavily on this one result though so they may be aware of this experiment’s limitations.
What's the relation of hair and immunosupression? The first successful immunosuppressed mice just happened to be nude?
Didn't know cancer could be so fussy!
I'm not quite sure. The mutation that leads to this strain of mice inhibits the development of the Thymus which is responsible for T cell production. Maybe the thymus is also necessary for hair growth?
It's also possible that the mutation affects a basic developmental pathway influcencing multiple aspects of development and the two most noticeable phenotypes are hair loss and immunosupression.
I upvoted your post.
Best regards,
@Council
Posted using https://Steeming.com condenser site.
Thanks
Upvoted.
DISCLAIMER: Your post is upvoted based on curation algorithm configured to find good articles e.g. stories, arts, photography, health, etc. This is to reward you (authors) for sharing good content using the Steem platform especially newbies.
If you're a dolphin or whales, and wish not to be included in future selection, please let me know so I can exclude your account. And if you find the upvoted post is inappropriate, FLAG if you must. This will help a better selection of post.
Keep steeming good content.
@Yehey
Posted using https://Steeming.com condenser site.
Can't argue with that.
This post has been voted on by the steemstem curation team and voting trail.
There is more to SteemSTEM than just writing posts, check here for some more tips on being a community member. You can also join our discord here to get to know the rest of the community!
Always appreciate the support SteemStem!