Vascular #1 - Why my leg is so painful ?

Have you ever experienced extreme pain over your leg? Or at least knowing a relative or a friend with similar problem? There are so many possible diagnoses for leg pain alone. It could be prolonged standing, wear and tear, injuries on the joints/bones/muscles/tendon or even the soft tissue. What I’m going to discuss about in this blog is about a type of pain that is quite unique and this type of leg pain can be quite debilitating to the individual. Oh yeah, this type of pain has nothing to do with high-heels. Though seeing those models from Victoria’s Secrets struting on their towering heels seem excruciatingly painful.
I’m gonna talk about a type of pain that is called the Intermitted Claudication. The fancy term “intermittent claudication” is described as a type of pain that affects the muscles of the leg, usually the calves but it could also involve the thigh and buttock, which is induced by exercise or long distance walking and somehow relieved by resting. The term “intermittent” comes into the name of the symptom because of its reversibility upon resting. Claudication simply means limping as it comes from the latin word “claudicare”, which means “to limp”. My vascular lecturer told us a story regarding an ancient kingdom in the Europe. There’s this one girl called Claudius or something. Every student looks similar but to identify Claudius, their lecturer will ask them to walk. Claudius is the only girl who limps. An odd way to come up with a medical term huh.
Intermittent claudication affects up to 5% of the world population, 60 years of age and above. It is the most common manifestation of the peripheral arterial diseases. Peripheral means “outer”, as in the most distal part of the human body. Hence, peripheral arterial disease means conditions that affects the distal arteries of the human body. Since we are talking about the leg pain, the arteries involved are located within the legs.
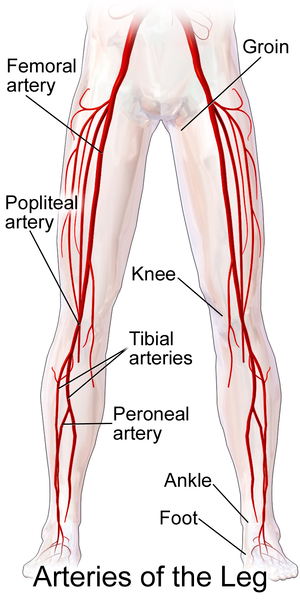
The location of the claudication may actually give a clue to the likely site of arterial disease. To know which artery is involved, it is vital to understand the anatomy of the arteries in the legs. The aorta that arises from the left heart descends to the abdomen and here it bifurcates into two common iliac arteries, which is the main supply of each leg. The common iliac artery gives of a branch to the internal iliac artery and the remnant part is the external iliac artery. The external iliac artery passes the inguinal ligament and becomes the common femoral artery which then subdivides again into the deep femoral artery and the superficial femoral artery. After the superficial femoral artery passes by the adductor magnus hiatus, it becomes the popliteal artery. Popliteal is the part located at the back of the knee. Popliteal artery continues its journey to the calves and give rise to the dorsalis pedis artery, peroneal artery, and posterior tibial artery.
After knowing the structures of artery in the lower limbs, we can somehow figure out which artery is the problematic one based on the location of muscle pain. Bilateral thigh or buttock pain could be caused by the aorto-iliac artery, unilateral thigh or buttock – iliac artery, calf – femoropoliteal artery, and foot – infrapopliteal tibial artery.
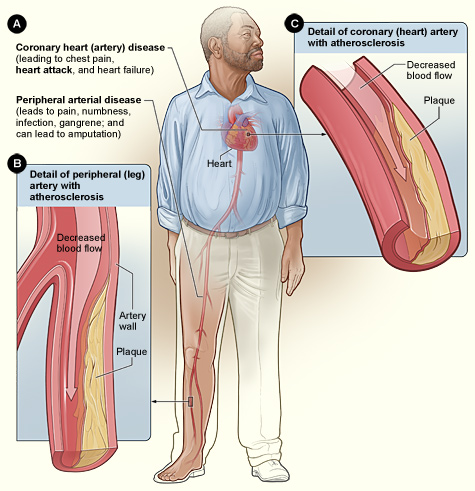
Peripheral arterial disease is caused by the atherosclerosis, for about 90% of patients. Yeah, there are so much co-morbids to be blamed in this condition. Smoking is one of the main risk factors that causes endothelial injury, which leads to atheroma and then plaque formation. Apart from that, abnormal blood cholesterol level and high blood sugar are some of the other risk factors to develop atherosclerosis. It can happen anywhere actually as long as there’s an artery running in it. If it involves the coronary artery, the patient can experience chest pain or heart attack. If the atherosclerosis involves the brain circulation, stroke can happen. If it involves those arteries in the kidneys, hypertension and even renal failure can develop. Such a widespread disease I must say. So let’s try avoiding excessive consumption of high fat, sugary foods and of course stop smoking.
So how does the pain develop?
So when the plaque obstructs the artery flow, the tissues those are supposed to receive blood supply do not actually get it. The pain is a result of reduced blood perfusion in the skin and the tissues underneath it. Take it as the dying nerves at that location screaming for help. It’s like those hungry chicks making noise while waiting for their mommy bird to feed them. Poor chicks.
Other features suggestive of claudication pain are the pain is not present at rest, comes on walking at a certain distance, quickly relieved by resting and it is repetitive in the sense that if the individual walks again at the same distance (claudication distance), the pain comes back again. Probably the first complain of the individual would be “I can’t go for window shopping anymore...”. Poor Susan.
Apart from arterial claudication, what other structures can cause claudication?
There are three typical culprits that cause leg pain, namely the arterial, neurogenic and venous types. To differentiate arterial and the other two causes, arterial pain results from the narrowing or occlusion of major lower limb arteries. In neurogenic pain, the nerves are to be blamed. Usually the lumbar nerve roots which supplies the lower limb are the source of the problem. Venous leg pain is caused by obstruction of the venous outflow of the leg, usually by deep venous thrombosis. Remember that the blood flows from the arteries, to the capillaries and finally reaching the veins?
The relieving features are somewhat distinct between those three types. For the arterial type, the pain usually vanishes after 1-2 minutes of resting. In comparison with the neurogenic type, the pain may gradually subside over 5-10 minutes. Lastly, venous pain usually requires the individual to elevate the leg to obtain relief. Why? It’s because that when the leg is raised, more blood will flow from the veins of the lower limbs to the heart. In standing postion, gravity pulls down the blood and causes difficulty for the veins to push the blood up to the heart. Elimination of gravity helps in this case, by raising up the leg.
The temperature of the legs might be different too. In arterial pain, the temperature could possibly be cooler as there is less blood flow to the limb. For neurogenic cases, the temperature is expected to be normal and in venous causes, the temperature might be increase due to the excessive blood pooling in the legs due to the venous insufficiency. Leg swelling is usually present in venous causes and absent in both neurogenic and arterial causes.
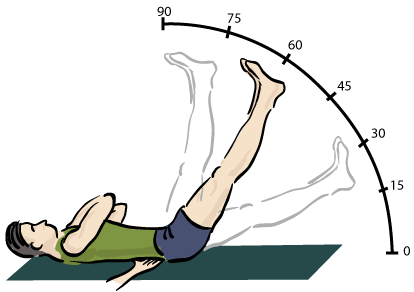
Finally, there’s a clinical test called the straight leg raising test that actually stretches the nerve and typically will cause pain if it is neurogenic in origin and the test is negative in both arterial and venous diseases. Oh yeah, the individual might complain of back pain too instead of just leg pain in neurogenic claudication.
Other facts about Intermittent Claudication?
- Only a small portion of affected individuals require revascularization surgery
- The mainstays of treatment are the risk factor modification (which I have mentioned earlier). Smoking cessation is vital as it is the main offender in this case. Exercise, statins (to reduce blood cholesterol level), oral hypoglycemic agents (to reduce blood sugar level) and antiplatelet therapy are recommended to control the disease.
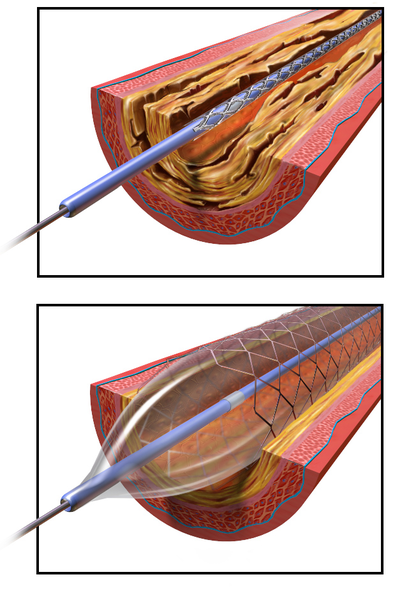
- Interventions in severe cases include the angioplasty, stenting and bypass surgery.
Intermittent claudication causes many problems on various aspects of one’s quality of life. Imagine that you are unable to do your daily routines like working and walking if you have this condition. The more important fact is that, intermittent claudication is actually a manifestation of peripheral vascular disease. People with this condition has a higher tendency to suffer from heart attack and stroke. Thus, if someone presented with leg pain, you should worry more about his/her heart and brain. Early diagnosis and commencement of the treatment mentioned above are the best way to avoid from getting more complications from this condition. So, stop reading this blog and start doing sit ups!
References
- Garden et al. Principles and Practice of Surgery. China. Churchill Livingstone. El Sevier, 2014. Print
- Intermittent claudication. the bmj. Retrieved on May 30, 2018, from https://www.bmj.com/content/333/7576/1002
- Leg Pain. Mayoclinic. Retrieved on May 30, 2018 from https://www.mayoclinic.org/symptoms/leg-pain/basics/causes/sym-20050784
- Intermittent Claudication. Wikipedia. Retrieved on May 30, 2018 from https://en.wikipedia.org/wiki/Intermittent_claudication

Congrats @soulesque
Your great article has been selected to feature in this week Air-Curation Round 15.
Expect an upvote from a supporter of this initiative.
Continue using the #Air-Cliniic tag.
Thank you :)
Hello @soulesque,
Air-Clinic sends her greeting! We are happy that you are creating amazing medical contents on Steemit using the #Air-Clinic tag.
This article was found as a result of #Air-Curie Initiative!We encourage you to keep it up!
Expect an upvote from @Air-Clinic soon!
If you haven't joined us on Discord please do so by clicking here
Cheers!
Dr. Qamran Bashir- Air-Clinic Curator!
My aunt said this leg surgery was more painful than her heart surgery. Great info @soulesque
Joy
Really huh. Thanks for the info :)