Pharmacology #4 : Exterminating the ever rampant Mycobacterium Tuberculosis
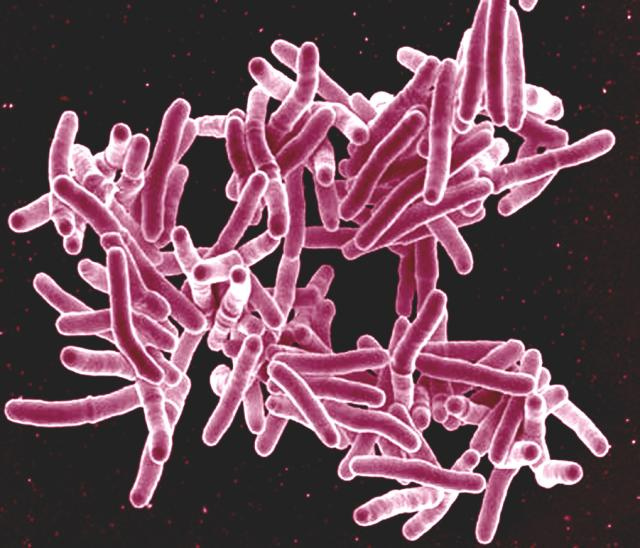
Mycobacterium tuberculosis is a part of the M. tuberculosis complex, the other members are Mycobacterium africanum and Mycobacterium bovis. More than 2 billion people are estimated to be infected by Mycobacterium tuberculosis. According to the World Health Organization, 1.7 million people has died in 2016 due to the infection. That shows how rampant this vile organism is.
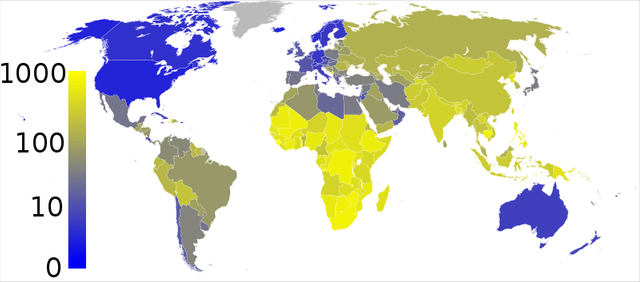
Higher rates of infection are epidemiologically situated in sub-saharan Africa, India, islands of South East Asia and Micronesia. Lower rates are found in the United States, Western Europe, Canada, Japan, and Australia. Poor socio-economy status, concurrent HIV infection and drug resistance are the major cause of the resurging TB epidemic.
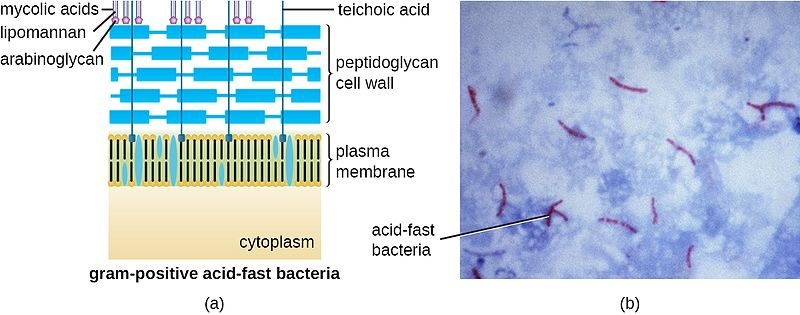
Mycobacteria are usually resistant to most antibiotics and because of their slow-growing nature, antibiotics those are active against rapidly growing organisms are useless to hinder this organism. The protective coat of the mycobacterium is impermeable to many antibiotics, thus it acts as a shield against typically used antibiotics. This makes the mycobacterium unique. Furthermore, mycobacteria resides in the macrophages, which is a type of white blood cell.
They are known to be intracellular organisms because of this special feature. Most drugs are incapable to penetrate the macrophages, making the mycobacterium safe and surrounded by a fortress made up of walls of macrophages. To further aggravate things, mycobacteria are notorious as they are brilliant enough to resist the actions of antibiotics. Hence, combination of many antibiotics is needed to arrest this vile creature. Unlike other types of infections which require a shorter course of antibiotics, anti-tb drugs require treatment that could cost up to months if not years.
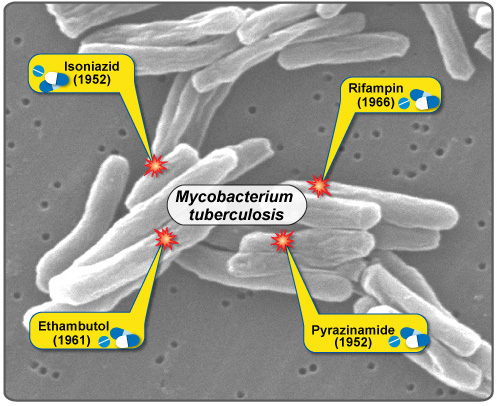
RIPES
RIPES is the mnemonic used to remember the first line antibiotics used to eradicate this organism. RIPES stands for:
R – Rifampicin
I – Isoniazid
P – Pyrazinamide
E – Ethambutol
S – Streptomycin
Among this five agents, Isoniazid and Rifampicin are the most active drugs. The combination of both rifampicin and Isoniazid has a cure rate up to 98%, after a 9 months period of therapy. The addition of the third agent, which is Pyrazinamide, further reduces the time required for the infection to be obliterated to 6 months without any loss of efficacy. In the current practice, 4 drugs are used to combat mycobacterium. The 4-drug regime comprises of Rifampicin, Isoniazid, Pyrazinamide and Ethambutol or Streptomycin. The choice of Ethambutol or Stremptomycin depends on the sensitivity testing from the mycobacterium culture results. Mycobacterium are usually cultured in liquid/broth in addition to a solid media (Lowenstein-Jensen slopes or Middlebrook agar). The liquid culture establishes the drug sensitivity result which takes approximately 3 weeks.
Neither Streptomycin nor Ethambutol adds to the efficacy of the 4-drug regime but they provide essential coverage if the organism resists Rifampicin, Isoniazid or both. In the United States, the prevalence of Isoniazid resistance is up to 10%. Thus, it is vital to add up till 4 drugs in the regime.
Isoniazid
Isoniazid is known to be the most active drug to treat tuberculosis and the structure is quite similar to Pyridoxine. Pyridoxine is Vitamin B6 and it is required by our body. You’ll see why this fact is important later. Isoniazid is less active against atypical mycobacterium species. This drug also has the capability in penetrating macrophages, hence making it potent to eliminate the bacteria.
How does Isoniazid works?
This antibiotic inhibits the synthesis of mycolic acid. Mycolid acids are the main ingredient that makes up the wall of mycobacterium. Halting the construction of the mycobacterium cell wall causes it to be weaker than usual. Drug resistant variants usually exists in the mycobacterial population at about 1 bacillus in 106. Classic tuberculous lesions often contain more than 108 bacilli. Hence, there are higher probability for the evil variant to exist, making the single drug therapy a poor choice.
Clinical Use
The RIPES treatment is recommended up till 6 months. Isoniazid may be used twice-weekly dosing regimen alongside other RIPES members. Isoniazid is usually given by the mouth. Supplement Pyridoxine is recommended too as the body will perceive Isoniazid as Pyridoxine, causing more of the vitamin to be removed from the body to avoid “toxicity”.
Adverse Reactions
Immunologic reactions such as fever and rashes are occasionally seen and in some cases, drug-induced SLE has been reported before. Direct toxicity of Isoniazid causes hepatitis, which is the inflammation of the liver. The liver enzymes tested in the liver function test can rise up till 3-4 times of the usual amount. The resultant hepatitis causes the person to develop nausea, vomiting, jaundice (yellowish discolouration of the skin and mucosa), and abdominal pain. Like I have mentioned earlier, Pyridoxine is excreted more from the body when Isoniazid is administered. Thus our body will suffer the deficiency of the Vitamin. Low amount of Vitamin B6 in our body causes peripheral neuropathy (numbness and weakness on our extremities).
Rifampicin
Rifampicin is produced by the bacteria Streptomyces mediterranei . This drug is able to combat other organisms such as groups of gram positive, gram negative cocci, some enteric bacteria, and chlamydia.
How does Rifampicin works?
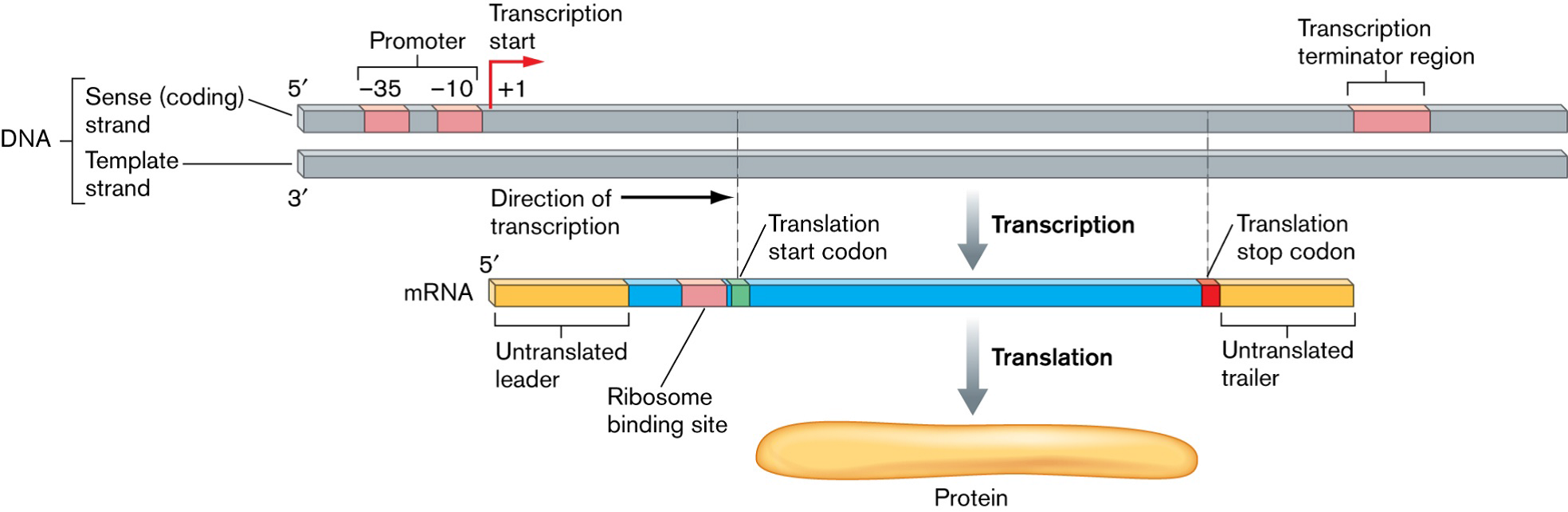
This drug binds to the B-subunit of bacterial DNA-dependent RNA polymerase. RNA polymerase promotes RNA synthesis, which aids in protein synthesis of the bacteria. Protein synthesis is important as the bacteria needs protein to survive. By blocking the RNA polymerase, the protein synthesis process is halted causing the mycobacteria to die. However, some mycobacteria mutants resist this drug in about 1 in 106 bacilli. These mutations result in poorer binding of rifampicin to RNA polymerase, making the drug useless. Similar to Isoniazid, this drug can enter macrophages easily. Making it superior to other antibiotics in combating Tuberculosis.
Clinical Use
Rifampicin is usually given 600mg daily or twice weekly for 6 months along with the other RIPES member. Apart from treating TB, this drug has some actions against Haemophilus influenza type B thus it can be given to treat the infection especially among children.
Adverse Reaction
Rifampicin discolours the urine, sweat and tears to orange. It is harmless though. Other side effects include rashes, low platelet count and inflammation of the kidneys.
Pyrazinamide
This drug is a relative to nicotinamide. It is inactive in neutral pH but in acidic pH, it exhibits its strength to combat the bacilli. Pyrazinamide is taken up by the macrophages too. It combats the mycobacteria within the acidic environment of lysozyme.
How does Pyrazinamide works?
Mycobacterium converts pyrazinamide to pyrazinoid acid. This acid disrupts the cell membrane of the mycobacteria and causes havoc to the transport functions within the cell wall. Resistance to this drug can happen when there is an impairment in the uptake of this pyrazinamide by the mycobacterium.
Adverse Reactions
The major side effect of this antibiotic include hepatotoxicity, causing liver impairment. Other effects include nausea, vomiting, fever and hyperuricemia. Hyperuricemia can provoke Gout.
Ethambutol
This drug is synthetic, water-soluble and heat stable.
How does this Ethambutol works?
This drug inhibits mycobacterial arabinosyl transferase. Arabinoglycan is one of the main part of the mycobacterial cell wall. Halting the enzyme arabibosyl transferase causes fewer arabinoglycan to be produces, making the cell wall weaker.
Clinical Use
This drug accumulates in individuals with renal failure and this drug also crosses the blood brain barrier. Ethambutol is usually given with the other first liners and can be given 50mg/kg twice-weekly.
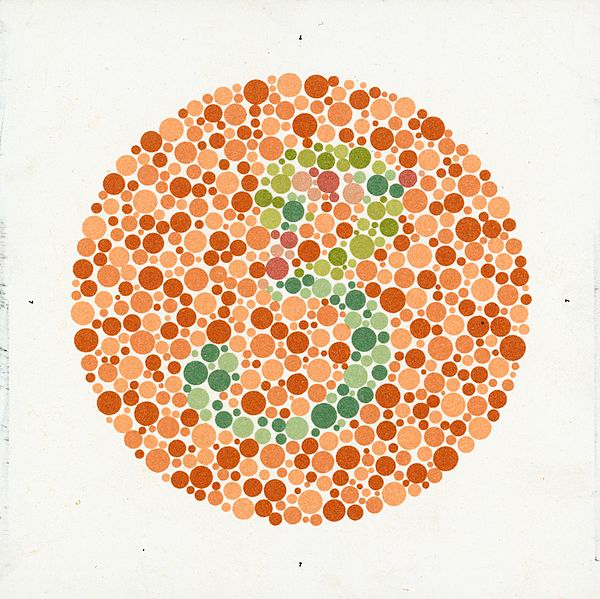
Adverse reactions
The most common side effect of this drug is retrobulbar neuritis. It is the inflammation of the retrobulbar nerve causing impairment in the individual’s visions and red-green colour blindness. Hence it is important to send the patient for Ophthalmologist follow up before and after commencing the therapy.
Streptomycin
Steptomycin was isolated from a strain of bacteria known as the Streptomyces griseus .
How does Streptomycin works?
This antibiotic is an irreversible inhibitors of protein synthesis. Non-tuberculous mycobacteria apart from Mycobacterium Avium Complex (MAC) and Mycobacterium kansasii are resistant against the actions of Streptomycin. In average, 1 in 108 bacilli are resistant towards streptomycin. Compared to the other anti-tb drugs, streptomycin poorly penetrates into the cells. Thus, it is only active against extracellular tubercle bacilli. Streptomycin too penetrates the blood brain barrier, making it useful to treat TB meningitis (TB causing inflammation to the meninges layer of the brain).
Clinical Use
It can be administered via intramuscular injection or via an intravenous line.
Adverse reaction
Streptomycin, similar to other aminoglycosides, are ototoxic and nephrotoxic. It means that they can harm the ear and the kidneys. Vertigo and hearing loss are one of the commonest side effect of streptomycin use and it may be permanent. The toxic effect of this antibiotic can be reduced by limiting the therapy no longer than 6 months.
Second Line antibiotics to treat tuberculosis are only taken to consideration when the Mycobacterium in the person is resistant towards the first line agents or in cases where there is no response after the RIPES treatment. Antibiotics indicated in this case are Ethionamide, Capreomycin, Cycloserine, Aminosalicylic Acid, Kanamycin, Amikacin, Fluoroquinolones and some others.
Alright, so those are the antibiotics require to eradicate the organism from the infected individual. Apart from that compliance to the medication very important and the Directly-Observed Therapy (DOT) is the mainstay method to ensure compliance to the medications. Patients need to take 4 different drugs for 6 months, thus I’m pretty sure that patients are prone to skip or not take the drug at all. This makes the annihilation process either prolonged, or useless. In short, research should be done to introduce better antibiotics to treat the infection. Preferably with lesser side effect and shorter course. Taking 4 drugs for many months is not an easy feat at all especially for those individuals with other co-morbidities such as Diabetes, Hypertension, Dyslipidemia and others as they are often supplied with ample of drugs to control their pre-existing diseases. With that thank you for reading :)
References
- Katzung et al. Basic & Clinical Pharmacology .Singapore: McGrawHill, 2012. Print
- Kumar P., Clark M., Kumar & Clark's Clinical Medicine. Ninth Edition. London: ElSevier, 2017. Print
- Epidemiology of tuberculosis. Uptodate. Retrieved on May 21, 2018, from https://www.uptodate.com/contents/epidemiology-of-tuberculosis
- Dheda K, Barry CE 3rd, Maartens G. Tuberculosis. Lancet 2016; 387:1211.
- Global Tuberculosis Report 2017. World Health Organization. Retrieved on May 21, 2018, from http://www.who.int/tb/publications/global_report/en/
- WHO Tuberculosis Programme-Framework for Effective Tuberculosis Control. WHO. Retrieved on May 21, 2018, from http://www.who.int/tb/publications/1994/en/index.html


Congratulations @soulesque! You have completed some achievement on Steemit and have been rewarded with new badge(s) :
Click on any badge to view your own Board of Honor on SteemitBoard.
For more information about SteemitBoard, click here
If you no longer want to receive notifications, reply to this comment with the word
STOPYou've been upvoted by TeamMalaysia Community :-
To support the growth of TeamMalaysia Follow our upvotes by using steemauto.com and follow trail of @myach
Vote TeamMalaysia witness bitrocker2020 using this link vote for witness