Microbiology #1 : The Notoriously Pathogenic Mycobacterium tuberculosis and its Mycolic Acid fortress

Once known as the White Plague , the first ever tuberculosis infection is thought to be as long as 9 000 years ago. Scientists were able to recreate genomes of mycobacteria from the 1 000 year old skeletal remains in southern Peru. Seals are the animal to be blamed for the migration of tuberculosis from Africa to South America as the human strain of tuberculosis is closely related to the mycobacterial species in the seals. Domesticated animals such as cows and goats contracted tuberculosis in Africa and then the seals came to the African beach to breed, which then gotten the infection. The seals migrated across the Atlantic Ocean and brought the vile mycobacteria alongside with them. The very first tuberculosis spread via human beings i thought to be in the trade routes of the old world.
Back in the Egyption glorious era, some of the mummies’ death were attributed to Mycobacterium tuberculosis . It was only at the end of the 19th century that Robert Koch first isolated Mycobacterium tuberculosis and postulated that this sinister being is the cause of the ever rampant Tuberculosis.
Mycobacterium is a genus of Actinobacteria , which belongs under the gram positive bacteria group. There is about 190 known species of mycobacteria worldwide. Mycobacteria came from the Greek prefix myco-, which means fungus. They are called as such because they exhibit similar mold-like fashion growth on the surface of the cultures. They are aerobic and non-motile with the exception of the Mycobacterium marinum species which has proven to be quite motile within the macrophages. They are capsulated and do not form endospores like fungi. The significant difference between Mycobacterium and other bacterias are the cell wall. Their cell walls are thicker, more hydrophobic, waxy and rich in mycolic acids. A polysaccharide, known as arabinogalactan holds the hydrophobic mycolate and peptidoglycan layers. Most antibiotics that show disruptive properties to the Mycobacterium tuberculosis species such as Rifampicin and Isoniazid, target the biosynthetic pathways of this cell wall formation.
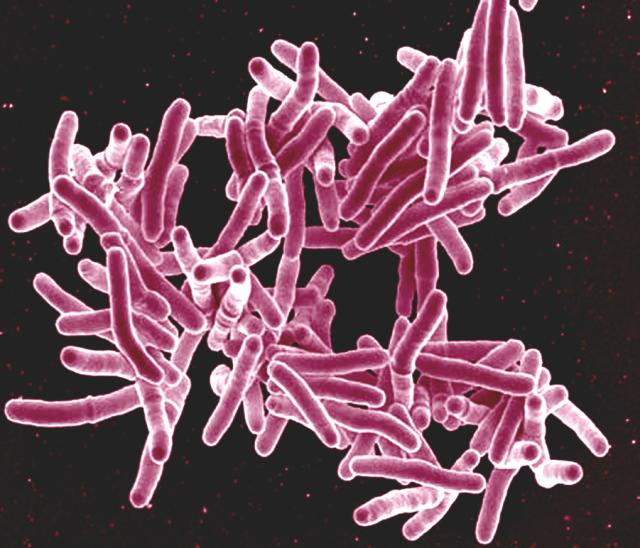
Microscopic observation of this species reveals a rod-shaped (hence the term bacilli) bacterium with 2-4 micrometer in length and 0.2-0.5 in width. The outmost layer of the bacteria is called the capsule and it is formed mostly of glycans. Underneath the capsule, there are layers of lipids called the mycolic acid decorated with porins and attached to another layer of sugary arabinogalactan. They can be classified under the gram positive bacteria category but they do not stain like them. Mycobacteria typically inhabits the water and food sources. This is true for most Mycobacteria but for those medically important mycobacteria such as the Mycobacterium tuberculosis and Mycobacterium leprae are obligate parasite and do not found elsewhere apart from the host’s body.
What makes Mycobacterium tuberculosis a worldwide pathogen?
Mycobacterium tuberculosis is an excellent pathogen with many features that distinguished it from the other bacteria. The success of this organism as a pathogen is mainly due to its insensitivity to most antibiotics and its capability to shield itself from the human immune response. As I’ve mention earlier, Mycobacterium tuberculosis is a fortress and its wall is made up of mycolic acid. It is very thick and impermeable to numerous chemicals. The complex cell wall composition alongside with efflux mechanisms and coated with numerous antibiotic degrading enzymes make it impermeable against antiobiotics such as B-Lactam, tetracyclin, fluoroquinolones, aminoglycosides and others. In order to combat this organism, multiple drug regime is indicated to eradicate this organism. I’ve written the mechanism of action of anti-tuberculous drugs in my previous post. Check it out.
Mycobacterium is known to be acid fast. What does it mean by this?
Acid fastness properties are described by their resistance to decolorization by acids during laboratory procedures. The acid-fastness of this mycobacterium is due to the high mycolic acid content in their cell walls. They absorb poorly and have a very high retention rate.
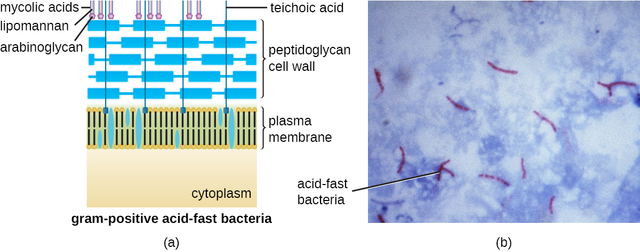
Mycolic acids or Mycolates are long fatty acid found in the cell walls of Mycobacteria. These acids comprise of a longer beta-hydroxyl chain and a shorter alpha-alkyl side chain. For instance, Mycobacterium tuberculosis synthesized three main types of chains, namely the alpha-, methoxy-, and keto-. 70% of the mycolic acids are made up of the alpha part and the remaining 30% originates from the methoxy- and keto- groups. Mycolic acid is the main culprit that halts typical antibiotic actions. This acid renders the antibiotics useless as it helps the mycobacterium to be more chemically and dehydration resistant.
To aggravate things, this mycolic acid allows the notorious Mycobacterium tuberculosis to dwell inside a macrophage. This fact further aids the isolation of Mycobacterium from the human immune response. There are five distinct stages of mycolic acid synthesis:
- C26 saturated straight fatty acids synthesis by the enzyme fatty-acid synthase to generate the alpha-alkyl branch of mycolic acids
- C56 fatty acids synthesis by the enzyme fatty-acid synthase-II to construct the meromycolate backbone.
- Cyclopropane synthases introduce functional groups to the meromycolate backbone
- The action of polyketide synthase Pks13 which condense the alpha-branch and meromycolate chain and further aided by the actions of corynebactericiae mycolic reductase A (CmrA) to finally establish the mycolic acid
- The actions of antigen 85 complex to transfer mycolic acid to the arabinogalactan.
So how does mycolic acid clinically relevant?
Staining process via some reagents are important to prove the presence of Mycobacterium in the person’s sputum. After the staining process, the slide is viewed under the microscope to observe the presence of this naughty bacilli. Stains to evaluate tissue specimen that contains mycobacterial species are the Ziehl-Neelsen stain, Kinyoun stain, and the Auramine Stain.
Ziehl-Neelsen Stain
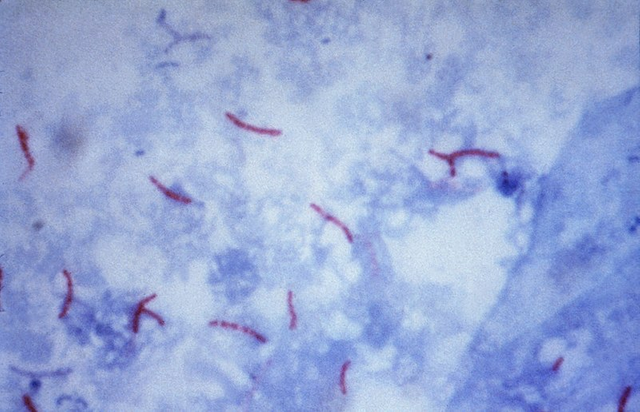
This staining procedure was first described by two German doctors: the bacteriologist Franz Ziehl and pathologist Friedrich Neelsen. The Acid-fast Bacilli (AFB) staining procedure involves the placement of the cells suspension onto a slide. The cells taken are usually from the patient’s sputum or phlegm. The liquid is air-dried and heated. After that, the slide is flooded with Carbol-Fushin. Carbol-Fushin is a mixture of phenol and basic fushin, which have better solubility in the thick cell wall lipid layer compared to the usual acid alcohol. After the flooding process, the slide is then rinsed and heated to dry. Isopropyl alcohol or methanol is added to remove the carbol-fushin back. Hence, cells which do not retain the carbol-fushin will be decolorized. Mycobacteria which have the mycolic acid retains the colour of carbol-fushin (red). After this procedure, the cells are flooded with methylene blue which acts as a counter stain. Non acid-fast bacilli will take up the methylene blue colour and becomes blue. Hence, there will be a striking difference between the mycobacteria species (Red) and other bacteria (blue).
Culturing Mycobacterium
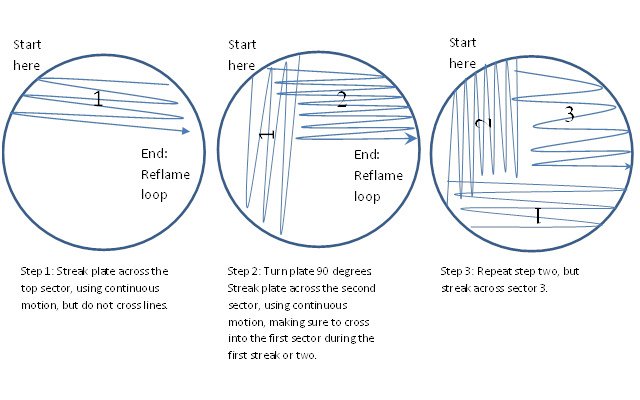
Individual bacteria placed in the agar will flourish into colonies and each clone is genetically identical to the primary ancestor introduced in the agar plate. Several methods are available to plate out the cells and one of the common technique used is streaking. This technique is commenced with a drop of culture on the end of a sterile loop of wire (inoculator) and it is streaked across the surface of the agar leaving the organism in the media. It is easily postulated that the initial streak has a higher amount of organism compared to the end. Agar plates maybe permissive or restrictive to the target organism, depends on the medical use. Example of agar that permits the multiplication of various organisms are the chocolate agar and selective ones (which only permits certain organism) are the Lowenstein-Jensen (which will be discussed further later) and Thayer-Martin agar (for Neisseria species).
Mycobacterium only flowers in rich media and multiplies every 16-20 hours, which is sluggish as compared to other bacteria. A prominent example is the Escherichia coli which grows every 20 minutes. Mycobacteria are aerobic as they require oxygen to flourish and forms rough, wrinkled colonies on solid culturing media.
The most famous media to cultivate Mycobacterium tuberculosis is the Lowenstein-Jensen medium. It is a type of selective media that promotes growth of this Mycobacteria. It contains malachite green, glycerol, asparagine, coagulated eggs, potato starch, and mineral salts such as potassium hydrogen phosphate, magnesium sulphate, and sodium citrate. The medium is green and opaque. The inclusion of some antibiotic such as penicillin and nalidixic acid in the media is to suppress the growth of other gram positive and gram negative bacteria which further enhance the proliferation of the Mycobacteria, as in less competition and crowd. Malachite green’s presence is also to restrain the growth of other bacteria. Glycerol acts as a nutrition supply to the Mycobacteria species.

The Middlebrook broth is a liquid growth medium for cultivating Mycobacterium tuberculosis and acts as an alternative to the Lowenstein-Jensen medium. It contains the ammonium sulphate, L-glutamic acid, sodium citrate, pyridoxine, biotin, disodium phosphate, monosodium phosphate, ferric ammonium citrate, magnesium sulphate, calcium chloride, zinc sulphate and copper sulphate. Cultures should be observed within 5-7 days after inoculation and once a week thereafter up to 8 weeks.
What are other types of Mycobacteria apart from Mycobacterium tuberculosis ?
Tests can be used to separate different groups of Mycobacteria. Before this, they are distinguished based on their growth rate and appearance. For example, M. leprae may take more than 20 days to multiply. Currently, the method used to identify strains of Mycobacteria are based on the alignment of core genomes of 57 strains of bacteria.
Mycobacterium Tuberculosis complex (MTBC), Mycobacterium avium complex (MAC) and Mycobacterium kansasii clade are some of the examples of slow growing Mycobacteria. Other types of Mycobacteria are not that popular as compared as those I’ve mention earlier hence I’ll only discuss those which are medically important.
MTBC or Mycobacterium Tuberculosis complex are genetically related group of Mycobacterium species which is known to cause tuberculosis in humans and animals. Examples of members in this group are:
Mycobacterium tuberculosis, Mycobacterium africanum, and Mycobacterium bovis.MAC or Mycobacterium Avium complex is another subtype of Mycobacteria that causes infection to the human especially in those infected with HIV. They are opportunistic infection that thrives on people with poor immune system.
The role of Mycobacterium bovis in immunization
Over a hundred years ago, two scientist from France began to culture species of mycobacterium that causes tuberculosis in livestock, named Mycobacterium bovis (AKA Bovine). The vaccine was named bacillus Calmette-Guerin (BCG) after its inventors and remains as the only licensed vaccination against tuberculosis. According to some clinical trials, BGC vaccination is capable of preventing to a whooping amount of 80% of adult TB cases as well as other various forms of TB in children and infants.
The first BCG vaccine was used medically in the year of 1921. As for 2004, the vaccine is given to approximately 100 children per year globally. One dose of BCG is recommended in healthy infants as close to their time of birth. BCG also has some protective properties against leprosy, Buruli ulcer and other non-tuberculous mycobacteria infections.
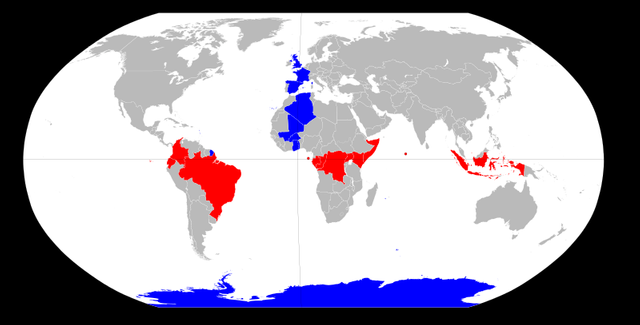
BCG vaccination is given intra-dermally (at the dermis, which is a layer of skin below the epidermis) usually at the deltoid region. A fascinating aspect regarding BCG is that, it tends to work better in countries further from the equator. Interesting right? Let’s just say that BCG vaccination does not work well in a sub-saharan African country such as Malawi but it excels in preventing tuberculosis in Europe.
In short, Mycobacterium tuberculosis brings tremendous impact towards the health of the world’s population. The powerful properties of this organism cause chaos to healthcare professionals and scientists as they are in a dire need of an ideal method to eradicate this organism. Currently, there are many ongoing and developing studies trying to develop the best therapeutic agent that will efficiently exterminate this organism from systems of the infected individuals. This can only happen if continuous financial support from various organization and the effort from the scientific community to study about this vile bacilli. Such developments are hope to happen in the near future :)
References
- Bowater L, et al. Microbiology Today - Mycobacteria. 2014 Society for General Microbiology. UK. 2014. PDF https://microbiologysociety.org/publication/past-issues/mycobacteria.html
- BCG Vaccine. Wikipedia. Retrieved on May 26, 2018, from https://en.wikipedia.org/wiki/BCG_vaccine
- Mycobacterium Tuberculosis. Bioquell. Retrieved on May 26, 2018, from http://healthcare.bioquell.com/en-us/resources-and-support/microbiology/mycobacterium-tuberculosis
- History of tuberculosis. Wikipedia. Retrieved on May 26, 2018, from https://en.wikipedia.org/wiki/History_of_tuberculosis
- Acid Fast Bacteria Culture. University of Rochester Medical Center. Retrieved on May 26, 2018, from https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=167&contentid=acid_fast_bacteria_culture
- Mycolic Acid. Wikipedia. Retrieved on May 26, 2018, from https://en.wikipedia.org/wiki/Mycolic_acid



Yeah, staining them is a PITA.
The slow growth rate has been postulated as to why it took so long for them to be isolated. A lot of plates are incubated for 24 to 72 hours. For a lot of bugs, this is a ton of doubling times (as in your E. coli example, this is 72 to 216 doublings - far enough time for visible colonies. For Mycobacterium, that could be as few as 6 doublings in about a week. We now think that earlier bacteriologists may have done everything right for isolation, but just simply assumed nothing was growing.
Thanks for the detailed info. They do grow very slowly huh. I bet this caused a lot of hassle especially to diagnose tuberculosis especially many years ago. Staining works but I don't think the sensitivity rate is as high as culturing. Furthermore, we need the culture results for the antibiotics susceptibility testings as some mutated strains are resistant to certain common anti-tb drugs.
Tuberculosis is a great menace in our world. Since it is air-borne, It is one of the high priority disease that scientist are working on inorder to control the spread.
In my country, TB Patients are paid a particular stipend to confine and also encourage them to eat well so that they can use their drugs.
The rate of transmission here is alarming
Thanks for putting together such a detailed article
Compliance is a huge issue because of the number of medication that the patients need to take to cure himself from tuberculosis. Tuberculosis is quite endemic in our areas right? as we are so close to the equator. Thanks for the nice words :)
This post has been curated by TeamMalaysia Community :-
To support the growth of TeamMalaysia Follow our upvotes by using steemauto.com and follow trail of @myach
Vote TeamMalaysia witness bitrocker2020 using this link vote for witness