Hematology #1 : The Coagulation Cascade

Bleeding is very common. I bet most people had some bleeding episodes at least once in a few months’ time regardless the location (gum, skin, nose, and others). The medical term for bleeding is Hemorrhage. I’m going to use this term later on, so please bear in mind. Hemorrhage is defined as blood escaping from the circulatory system, which means from the blood vessels.
In normal situation, the lining of the blood vessels contains anti-coagulants, circulating platelets and clotting factors. The anti-coagulant stops any coagulation process without any triggers. You don’t want your blood to clot randomly without any triggers right. In some diseases that cause any defect to the anticoagulants, the blood might clot randomly and it is important to take some medications that stops blood coagulation. In the setting of any injury, the environment becomes more pro-coagulant – as in the area becomes suitable for coagulation to happen. Injury activates proteins such as collagen and von Willebrand factor which results in platelet activation.
What are platelets?
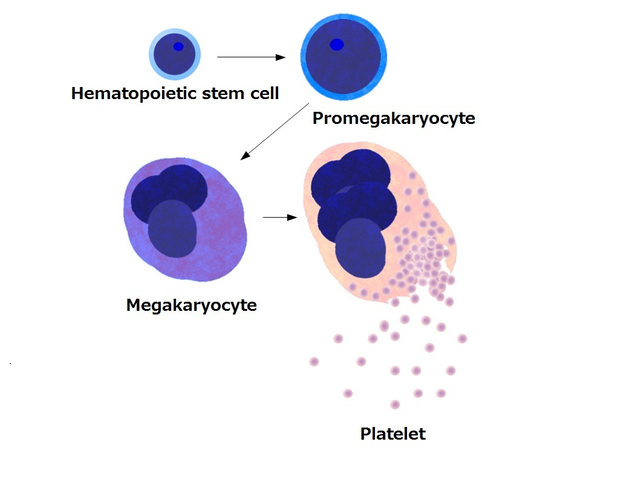
Platelets are known as thrombocytes and contains no cell nucleus. They are derived from the big group of megakaryocytes which originates from the bone marrow, similar to the red blood cells and white blood cells. The primordial form of platelet is the myeloid stem cell. They exist in the bloodstream as biconvex (lens-shaped) structure and their diameter is about 2-3micrometer. The structure of platelets include the GP Ia, GP Ib, GP IIb, and GP IIIa. I’ll explain about these receptors shortly later. Low platelet count in the blood test (Full Blood Count) is known as Thrombocytopenia and high platelet count is termed as Thrombocytosis . They are mainly involved in the blood clotting process as in when there’s any injury to the skin or blood vessels, they are activated and forms blood clot to plug in the leaked vessels. Hence, blood will stop flowing or leaking from the blood vessels. Thrombocytopenia is dangerous as when injury happens, the chances or the time taken for the blood to clot is increased which causes the blood to leak more.
Back to the injury response, platelets are activated and vasoconstrictors (substances that constricts the blood vessels) are secreted. After that, there will be more platelets recruitments. Within the platelet, thromboxane A2 (TXA2) is synthesized from arachidonic acid and it exerts its effect as platelet activator and potent vasoconstrictor. Platelets too release Adenosine DiPhosphate (ADP) which is a powerful inducer to platelet aggregation and as well as the hormone Serotonin (5-HT) is released which assists in aggregation and vasoconstriction. r
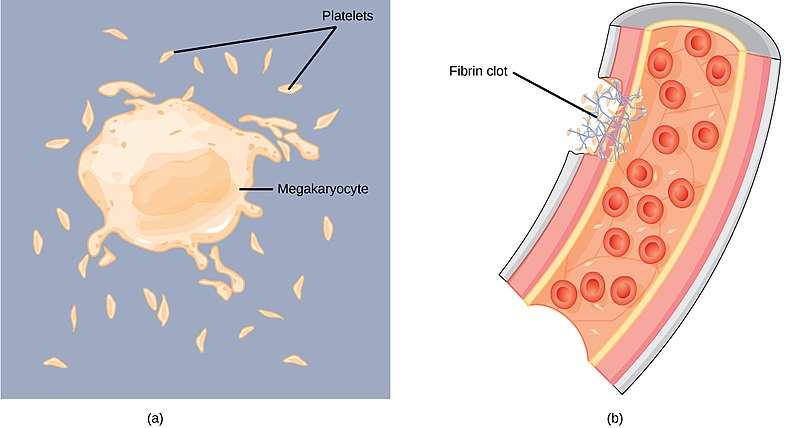
During an injury, Collagen binds to GP Ia receptor of the platelet and Von Willebrand Factor (vWF) binds to the GP Ib receptor. These will then trigger the release of TXA2, ADP and 5HT. I have mentioned about the effects of these substances before. The activation of platelet results in conformational changes in IIb and IIIa receptors resulting in to bind to fibrinogen. Simultaneously, the clotting cascade is activated and the outcome is thrombin production and a fibrin clot. Fibrinogen is converted to fibrin in the cascade and this fibrin clot stabilizes the platelet plug.
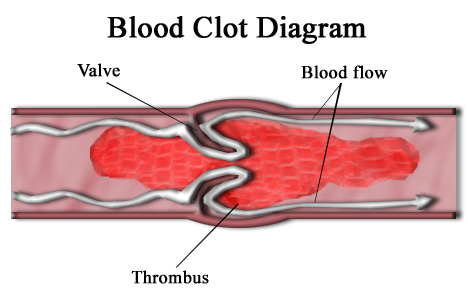
There are two types of thrombi or clots. White thrombi form in high flow rate and high shear force environment within the arteries. The name is as such because of its rich platelet content. These thrombi is dangerous as it will clog and plug the blood vessels, which lead to ischaemia (restriction of blood supply to the tissue) to the target organ. Just imagine that the blood supply to your toes is occluded because of this thrombi. Hence, there will no blood flow to supply oxygen and nutrients to your toes, resulting in Toe Ischaemia.
Blackened toe, yikes! Venous thrombi is recognized pathologically as the red thrombi because of its huge content of red blood cells. It can cause the affected limb to be painful and swollen (This condition is known as Deep Vein Thrombosis), but the most serious complication of this Red Thrombi is when it gets dislodge from your legs. After dislodging, it will travel to the heart via the inferior vena cava and then to the lungs. Then, it’ll get stuck to one of the pulmonary circulation which then will compromise breathing. The heart will try to compensate the poor breathing efforts, and this might result in heart failure and in worst case scenario, sudden death. This is known as Pulmonary Embolism.
Coagulation Factors
There are 13 clotting factors which are labeled in roman numerals.
I = One – Fibrinogen
II= Two - Prothrombin
III = Three – Tissue Factor
IV = Four – Calcium
V = Five – Labile Factor
VI = 6 - Accelerin
VII = 7 – Stable Factor
VIII = 8 – Anti-Hemophilic Factor A
IX = 9 – Christmas Factor
X = 10 – Stuart Power Factor
XI = 11 – Plasma Thromboplastin Antecedent
XII = 12 – Hageman Factor
XIII = 13 – Fibrin Stabilizing Factor
Each of the clotting factors have their own inactivated and activated form. The inactivated form, as the name implies, is not active. It means that it is in its dormant state. The active form of the factor has the letter “a” attached to it. For example, IIa and IIIa.
Coagulation cascade is one of the most complex thing that medical students have to memorize or at least understand. There are several clinical importance that this cascade exhibit. Some disease that is related to prolong bleeding can be due to the deficiency in any of this factors. Some drugs such as Warfarin and Heparin which are used to prevent Stroke has anti-coagulation properties and it plays a part by interfering with the cascade. I’ll explain that later. Let’s focus on the ways to remember about the cascade easily. I have retrieved this from a blog (which I have placed it at the reference list), and I find it quite easy to understand.
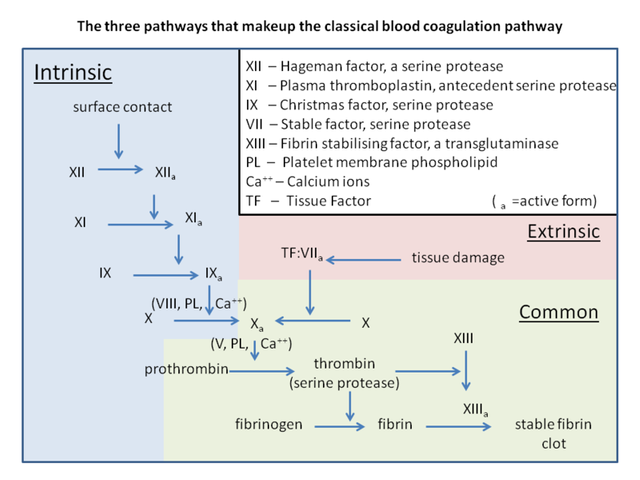
There are two initial pathways involving in the coagulation cascade: **Intrinsic pathway and extrinsic pathway.(( The final pathway is known as the common pathway which results from the activation of both intrinsic and extrinsic pathways. The main aim for this coagulation cascade is to generate fibrin as it will stabilize the platelet plug, sealing the injury site. All the clotting factors are synthesized in the liver with the exception of factor IV (calcium) and factor VIII carrier protein: vwF (Von Willebrand Factor)
The common pathway should be remembered with this mnemonic, 1 x 2 x 5 = 10. It involves factors I, II, V, and X. Easy right?
Intrinsic pathway involves clotting factors from XII to VIII excluding X because it is in the common pathway. So the factors involved are XII, XI, IX, and VIII. The descending order is used because the cascade begins with factor XII.
The extrinsic pathway is remembered as 3 + 7 = 10. Since 10 is a part of common pathway, then factors III and VII are involved in the extrinsic pathway.
How does Vitamin K involved in the pathway?
Vitamin K is one of the fat soluble vitamins that prerequisites the blood coagulation pathways. Vitamin K is mostly found in green leafy vegetables because it has direct involvement in photosynthesis. Factors II, VII, IX, and X are Vitamin K dependent coagulation factors as it need Vitamin K to be activated. Clotting factors in newborns are just around 30-60% of the adults’ normal Vitamin K value. Hemorrhagic Disease of the Newborn is caused by the lacking of this Vitamin. Deficiency in this Vitamin can result in hospitalization, blood transfusion and damage to the brain. Usually Vitamin K is injected in newborns to prevent the disease.
So what's the significance of knowing the clotting cascade?
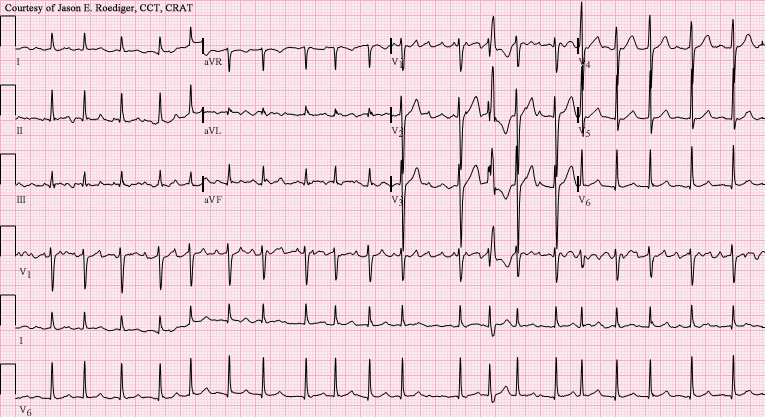
Liver diseases and Warfarin can affect the Vitamin K dependent coagulation factors. Since Tissue factor (Factor III) and Factor VII are involved, the extrinsic pathway is affected. This pathway is monitored by a blood investigation called the PT or Prothrombin Time. Normal PT value is about 12-16 seconds. INR or International Normalized Ratio is much common investigating method to look for the disruption of extrinsic pathway because it is basically Prothrombin time compared with a normal person. Hence, if the INR is elevated, that means the PT is prolonged, which is caused by some problems in the Extrinsic Pathway.
Anti-thrombin III is an endogenous anticoagulant and a member of the serine protease inhibitor. It inhibits factor IIa and factor X. The intrinsic pathway is affected in this case and thus, the blood investigation method involved is the aPTT (Activated Partial Thromboplastin Time). Any disruption to the intrinsic pathway causes prolonged aPTT. The normal aPTT value is 26-34 seconds. Heparin plays a part in this mechanism.
Proteins C and S are endogenous anticoagulants which attenuate the blood clotting cascade by proteolysis of the cofactors V and VIII. It is interesting to note that both of the factors mentioned have an identical overall domain structure and it is considered to be homologous. Since it is Vitamin K dependent and Warfarin (a vitamin K inhibitor) can inhibit these proteins C and S, cofactors V and VIII could be activated and causes the situation to be pro-coagulant in which Warfarin is trying to prevent. Hence, usually Warfarin is co-administered with Heparin for a few days to make this paradoxical situation unlikely.
Anticoagulants
I have explained about Deep Vein Thrombosis causing Pulmonary Embolism earlier. It’s basically a clot from your legs which then dislodges to your lungs and causes difficulty in breathing. It is a serious condition. The German physicist Rudolf Virchow (1821-1902) described the elements that makes up the famous Virchow’s Triad. This triad consists of hypercoagulability, hemodynamic changes (stasis) and endothelial injury. These triad of elements predisposes people to thrombosis. Hypercoagulability is a state where the environment becomes more suitable for coagulation such as in cases like Antiphospholipid syndrome. In this syndrome, there is inhibition of Protein C and Protein S. The inhibition causes the situation to be pro-coagulant (supports coagulation) and results in many problems such as miscarriage and even stroke. Stasis means a period of inactivity or in other terms, not moving or immobile.
The blood flow becomes slower and particles in the coagulation cascade tend to activate easily. The causes of stasis includes long surgical operation, prolonged sitting such as in long hours flight and varicose veins – in which there will be dilated and tortuous veins. Endothelial injury can arise from stress, infection or trauma which damages the endothelial lining of the blood vessels.
There are three main subtypes of anticoagulants
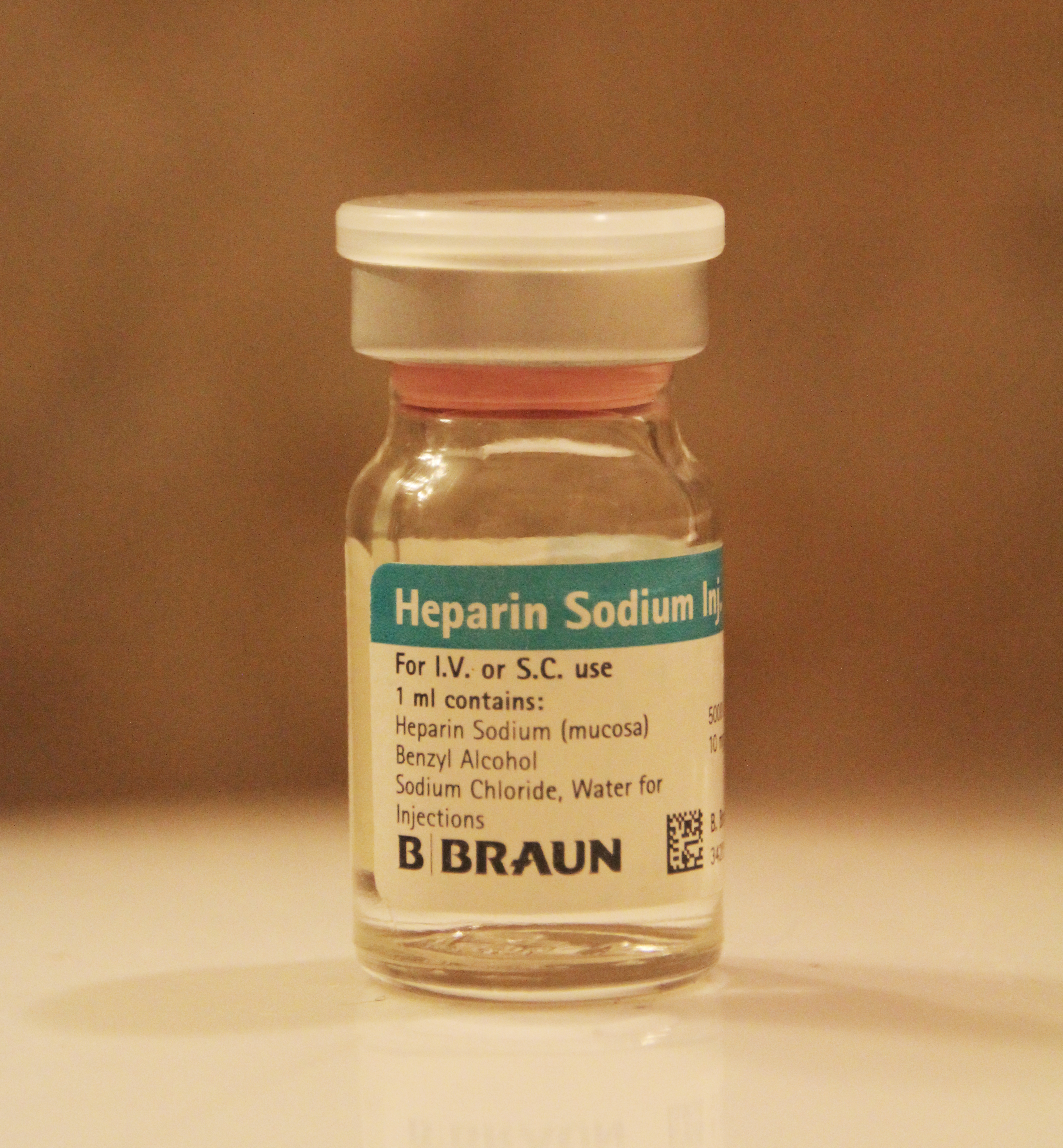
• Unfractionated Heparin
• Low Molecular Weight Heparin ( LMWH)
• Warfarin
Unfractionated Heparin
• This drug binds to the Anti-Thrombin III which then causes conformational change to its structure causing the inhibition effects to factors II, IX and X to be 1000-fold stronger. This significantly slows down the coagulation process and thus decreases the chance for blood to clot. As I have explained earlier, the action of this type of drug is measured via the aPTT (activated Partial Thromboplastin Time).
Low Molecular Weight Heparin (LMWH): Enoxaparin (Clexane), Dalteparin and Tinzaparin
• Similar to Unfractionated Heparin, it binds to the Anti-Thrombin. What makes it different is that it has little effect on Factor II (Thrombin). Since it does not affect Thrombin, the measurement of aPTT is seldom used to monitor this drug’s activity.
Heparin Toxicity
• Bleeding
• Heparin induced Thrombocytopenia
Warfarin

• The clinical use of Coumarin anticoagulant started with the discovery of an anticoagulant substance formed in spoiled sweet clover silage which causes hemorrhagic disease in cows. Warfarin’s name originates from the term Wisconsin Alumni Research Foundation and the “arin” part arises from the Coumarin group.
• It is one of the most commonly prescribed drugs as the users are approximately around 1.5 million individuals. The usual indication to prescribe this drug includes the prevention of clot formation in cases such as Atrial Fibrillation or Valvular Heart Disease. It can be given to prevent recurrent ischaemic stroke too.
• Warfarin, as I have mentioned earlier, inhibits the synthesis of Vitamin K dependent factors such as II, VII, IX, and X. There is an 8 hour to 12 hour delay in the action of this drug.
• Close monitoring is required as it exhibits dangerous side effects. The effects should be monitored via the INR (International Normalized Ratio). I have explained about it earlier.
Warfarin Toxicity
• It should never be administered in pregnancy as it can cross the placenta and affect the fetus.
• Bleeding, up to 3% of cases. The risk is further increased when it is combined with anti-platelet drugs such as Clopidogrel, Aspirin, or NSAIDs.
I hope this info help the science community of Steemit. For healthcare professionals, it's quite good to revise back about the cascade as numbers are difficult to memorize especially if you don't use it everyday. With that, have a good day :)
References
- Katzung et al. Basic & Clinical Pharmacology .Singapore: McGrawHill, 2012. Print
- Simple Coagulation Cascade with Mnemonics. EpoMedicine. Retrieved on April 24, 2018, from http://epomedicine.com/medical-students/simple-coagulation-cascade-mnemonics/
- The clotting cascade made easy. Blogging for your nogging. Retrieved on April 24, 2018, from http://epomedicine.com/medical-students/simple-coagulation-cascade-mnemonics/
- Vitamin K. Wikipedia. Retrieved on April 24, 2018, from https://en.wikipedia.org/wiki/Vitamin_K#Injection_in_newborns



I used to work for a medical company in Spain, at a national level, distributing a porcine factor VIII for patients with that kind of hemophiliac problem. Nice post, interesting and educative. Thank you
That's one of the most commonest blood factor deficiency disorder! Thanks for the support :)
Your Post Has Been Featured on @Resteemable!
Feature any Steemit post using resteemit.com!
How It Works:
1. Take Any Steemit URL
2. Erase
https://3. Type
reGet Featured Instantly & Featured Posts are voted every 2.4hrs
Join the Curation Team Here | Vote Resteemable for Witness
Wonderful article. I remember the time where I studied about coagulation cascade during my first year of medical school. Keep it up.
It's quite hard to remember because we don't use it on day to day basis. I hope this article helps as a refresher. Thanks for the support !
Interesting one @soulesque
You must have heard of clot-buster .... Its a licensed trade product and the protein was isolated from a Actinobacteria isolated from the hot spring water source.
I never heard of it but i will look for it. Thank you for the info !
This post has been curated by TeamMalaysia Community :-
To support the growth of TeamMalaysia Follow our upvotes by using steemauto.com and follow trail of @myach
Vote TeamMalaysia witness bitrocker2020 using this link vote for witness