Common STD - HPV
Loveful exaltation, contact between two bodies, mutual adoration. All of this ending in orgasm. All this means not only the harmony of hearts, but also pathological changes located within the anogenital area. One of signs that occurs in HPV infection is candyloma acumitum. When we do not cure them, There is a chance, that it will cause much bigger problem – tumor-like pathology named nodylomata gigantea Buschkhe-Lowewnstein.
HPV is a very common virus. More than 50% of sexually active people have in their blood antibodies against capsid proteins of the virus (Majewski S., et al., 2005)1. HPV isn’t just genital virus. It is quite common for this virus to appear in many parts of human body. We can find clinical evidence of HPV presence on our hands or feet. Obviously, oral cavity is also place which we use for sexual contact, hence we can find etiological factors typical for perineum there too. Also, we shouldn’t be surprised by HPV-dependent cancer in head and neck region (Kiwerska K., et al., 2012)2.
Transmission
It is estimated that we have 650 million people infected by HPV (Jach R., et al., 2008)3. Most common way that virus use to infect us, is sexual contact. Let’s expand it a little bit. Man have the most chance to being infected by anal sex (47,1 tr/p-m), and then vaginal sex (27,8 tr/p-m). In case of woman, the riskiest is anal sex (5,9 tr/p-m) and accidental contact of the scrotum with the female anus (6 tr/p-m) (Hernandez B., et al., 2008)4.
HPV can infect cells that possess an ability to multiply. This specific type of cells is located in the stratum basale, which is the deepest layer of the epidermis. Infected keratinocyte migrate to stratum corneum where virions are released. To transmit the infection, there must be a presence of pathological changes, which arise from biological activity of the virus, also the skin must be damaged, because this is the only way to spread HPV to the deepest epidermis layer.
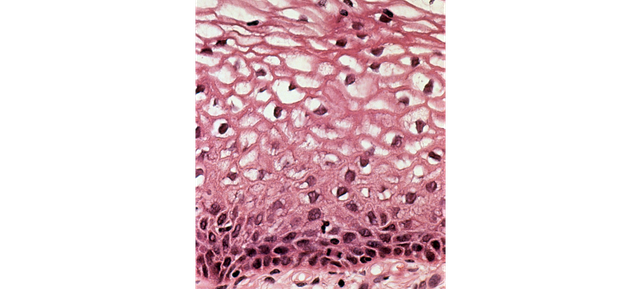
Figure 1 In the slide we can see squamous cells with a perinuclear empty cavity surrounded by cytoplasmic thickening and with nuclear enlargement. This view corresponds to koilocytes. License: CC0
Cervical cancer is strongly connected to HPV infection. This cancer is responsible for 266 000 deaths per year around the globe (Frumovitz M., et al., 2017)5. It is good to remember that we have something around 10 to 20 years between HPV infection and cancer. We can stand against this pathological process by gynecological examination and Pap test. It is simple to avoid this cancer via treatment or vaccination
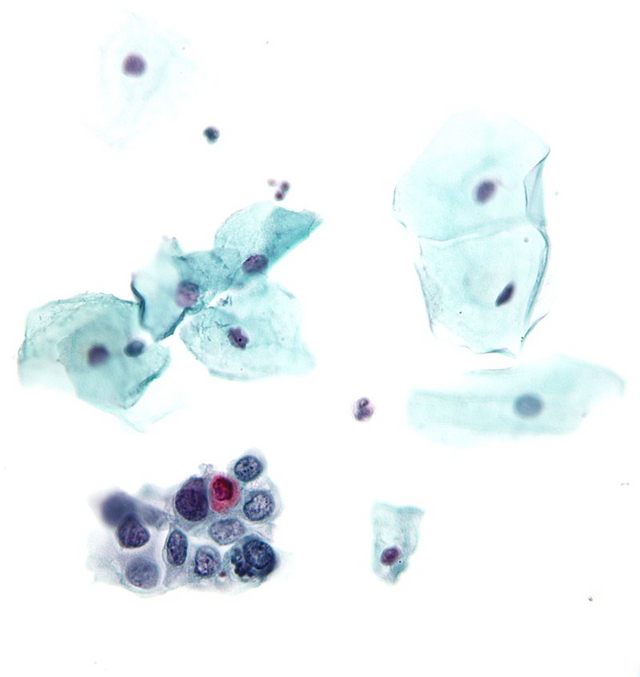
Figure 2. Pap test. On the bottom we can see small, round cells with irregular coarsely clumped chromatin. That kind of findings is typical to cervical intraepithelial neoplasia grade III. License: CC BY-SA 3.0
Vaccinations
Female population is not alone in HPV problem. Every sexually active person is in danger. This is why in the perfect world, we should vaccinate both men and women. In case when a public health care system is ineffective, girls should be prioritized for vaccination. There is a serious reason to do so. Before pubescence inside a cervical canal there is columnar epithelium, inside a vagina - stratified squamous epithelium, but transition zone between them does not exist. During sexual maturation, the columnar epithelium “fill” into vaginal part of the cervix. In this way, exposed cylindrical epithelium undergoes metaplasia and transition zone is developed. Time between eversion of endocervical epithelium from inside the endocervical canal onto the outside of the cervix is dangerous, because this kind of epithelium have different mechanical characteristics. It’s much easier to break the continuity of the columnar epithelium. If this happens, the virus has an open infection gateway. This theoretical knowledge is confirmed by epidemiology. Peek of the new case of HPV infection falls on female between ages of 18 and 25.
If we want to reduce spreading of HPV-infection we should vaccinate young people before sexual initiation. Protection against oncogenic types of HPV especially 16, 18, 31, 33 may lead to avoidance of cervical cancer in women case. In the case of men vaccines can reduce incidences of squamous cell carcinoma of the penis.
Effectiveness of prophylactic and therapeutic vaccinations has been shown in randomize and double-blind study. The bivalent vaccine resulted in a 91.6% decrease in the incidence of accidental infections, a 100% reduction in persistent infections, and a 93.5% decrease in cytological changes (Harper D.M., et all., 2004)6. Study named FUTURE II confirmed this finding. It is now believed that the widespread introduction of HPV vaccine will reduce the number of deaths from cervical cancer by 95%.
References:
1 Majewski S., et al., 2005
2 Kiwerska K., et al., 2012
3 Jach R., et al., 2008
4 Hernandez B., et al., 2008
5 Frumovitz M., et al., 2017
6 Harper D.M., et al., 2004
FUTURE II
This post has been voted on by the SteemSTEM curation team and voting trail in collaboration with @curie.
If you appreciate the work we are doing then consider voting both projects for witness by selecting stem.witness and curie!
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Congratulations @hitsug! You have completed the following achievement on the Steem blockchain and have been rewarded with new badge(s) :
Click here to view your Board of Honor
If you no longer want to receive notifications, reply to this comment with the word
STOPDo not miss the last post from @steemitboard:
Witaj.
Studiujesz medycynę?
Cześć. Tak. Zbliżam się do końca tej długotrwałej przyjemności