BMP-2, too much of a good thing?
BMP-2, too much of a good thing?
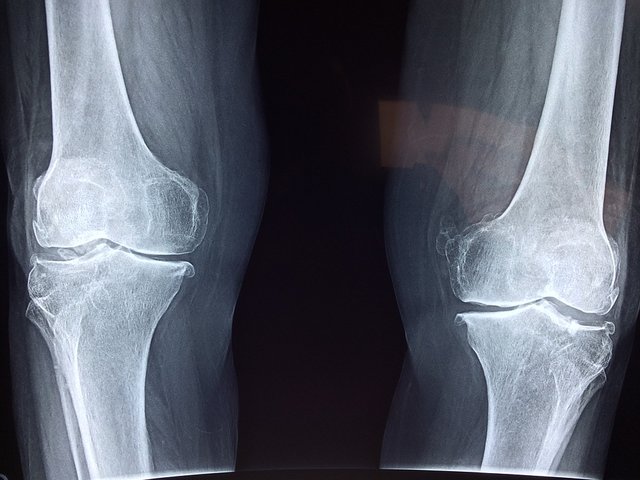
Image CCO Creative Commons
But let’s go in order and see how and when BMP-2 is used.

Image CCO Creative Commons
What are the side effects of BMP-2?
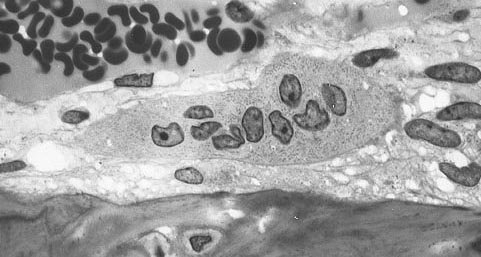
Image CCO Creative Commons
So while it is true that more bone is being produced as a result of BMP-2, this bone was found to be of poor quality and containing low mineral density (Aghaloo et al. 2007; James et al. 2012). Especially when used in spinal fusion surgeries, BMP-2 can have several side-effects, the worst one is probably ectopic bone formation that is caused by the leakage of BMP-2 outside the implant (James et al. 2016) . BMP-2 not only direct the differentiation of stem cells, but it can also change the phenotype of cells like myoblasts (Chen et al. 1998), adipocytes (Fraser et al. 2006) and fibroblasts (Ishihara, Weisbrode, and Bertone 2015) that inhabit the surrounding tissues, causing some problems. You don’t have to trust me on that, few years after the approval of BMP-2, the FDA issued a warning, urging clinicians to be careful with the use of BMP-2 because it was found that from 20 to 70% of the surgeries that used BMP-2 showed some sort of BMP-2-associated complications (Carragee, Hurwitz, and Weiner 2011). This data is often overlooked in scientific publications. With this article I don’t want to dispute the therapeutic benefits of BMP-2, probably to date we don’t have better alternatives, but I just wanted to highlight how sometimes we are biased in reporting facts.
References
Aghaloo, Tara et al. 2007. “A Study of the Role of Nell-1 Gene Modified Goat Bone Marrow Stromal Cells in Promoting New Bone Formation.” Molecular therapy : the journal of the American Society of Gene Therapy 15(10): 1872–80. http://www.ncbi.nlm.nih.gov/pubmed/17653100.
Carragee, Eugene J, Eric L Hurwitz, and Bradley K Weiner. 2011. “A Critical Review of Recombinant Human Bone Morphogenetic Protein-2 Trials in Spinal Surgery: Emerging Safety Concerns and Lessons Learned.” The spine journal : official journal of the North American Spine Society 11(6): 471–91. http://www.ncbi.nlm.nih.gov/pubmed/21729796.
Chen, D et al. 1998. “Differential Roles for Bone Morphogenetic Protein (BMP) Receptor Type IB and IA in Differentiation and Specification of Mesenchymal Precursor Cells to Osteoblast and Adipocyte Lineages.” The Journal of cell biology 142(1): 295–305. http://www.ncbi.nlm.nih.gov/pubmed/9660882.
Fraser, John K, Isabella Wulur, Zeni Alfonso, and Marc H Hedrick. 2006. “Fat Tissue: An Underappreciated Source of Stem Cells for Biotechnology.” Trends in biotechnology 24(4): 150–54. http://www.ncbi.nlm.nih.gov/pubmed/16488036.
Hori, Masateru et al. 2006. “Bone Morphogenetic Protein-2 Counterregulates Interleukin-18 MRNA and Protein in MC3T3-E1 Mouse Osteoblastic Cells.” Connective tissue research 47(3): 124–32. http://www.ncbi.nlm.nih.gov/pubmed/16753805.
Ishihara, Akikazu, Steve E Weisbrode, and Alicia L Bertone. 2015. “Autologous Implantation of BMP2-Expressing Dermal Fibroblasts to Improve Bone Mineral Density and Architecture in Rabbit Long Bones.” Journal of orthopaedic research : official publication of the Orthopaedic Research Society 33(10): 1455–65. http://www.ncbi.nlm.nih.gov/pubmed/25418909.
Itoh, K et al. 2001. “Bone Morphogenetic Protein 2 Stimulates Osteoclast Differentiation and Survival Supported by Receptor Activator of Nuclear Factor-KappaB Ligand.” Endocrinology 142(8): 3656–62. http://www.ncbi.nlm.nih.gov/pubmed/11459815.
James, Aaron W. et al. 2016. “A Review of the Clinical Side Effects of Bone Morphogenetic Protein-2.” Tissue Engineering Part B: Reviews 22(4): 284–97. http://online.liebertpub.com/doi/10.1089/ten.teb.2015.0357.
James, Aaron W et al. 2012. “Perivascular Stem Cells: A Prospectively Purified Mesenchymal Stem Cell Population for Bone Tissue Engineering.” Stem cells translational medicine 1(6): 510–19. http://www.ncbi.nlm.nih.gov/pubmed/23197855.
Keating, J F, A H R W Simpson, and C M Robinson. 2005. “The Management of Fractures with Bone Loss.” The Journal of bone and joint surgery. British volume 87(2): 142–50. http://www.ncbi.nlm.nih.gov/pubmed/15736731.
Robin, Brett N et al. 2010. “Cytokine-Mediated Inflammatory Reaction Following Posterior Cervical Decompression and Fusion Associated with Recombinant Human Bone Morphogenetic Protein-2: A Case Study.” Spine 35(23): E1350-4. http://www.ncbi.nlm.nih.gov/pubmed/20938385.
Shahlaie, Kiarash, and Kee D Kim. 2008. “Occipitocervical Fusion Using Recombinant Human Bone Morphogenetic Protein-2: Adverse Effects Due to Tissue Swelling and Seroma.” Spine 33(21): 2361–66. http://www.ncbi.nlm.nih.gov/pubmed/18827703.
Spadaro, Joseph A., Robert O. Becker, and Charles H. Bachman. 1970. “The Distribution of Trace Metal Ions in Bone and Tendon.” Calcified Tissue Research 6(1): 49–54. http://link.springer.com/10.1007/BF02196183.
Urist, M R. 1965. “Bone: Formation by Autoinduction.” Science (New York, N.Y.) 150(3698): 893–99. http://www.ncbi.nlm.nih.gov/pubmed/5319761.
Zara, Janette N et al. 2011. “High Doses of Bone Morphogenetic Protein 2 Induce Structurally Abnormal Bone and Inflammation in Vivo.” Tissue engineering. Part A 17(9–10): 1389–99. http://www.ncbi.nlm.nih.gov/pubmed/21247344.
Communities that support me are:
Image created by @gtg
IMMAGINE CC0 CREATIVE COMMONS, si ringrazia @mrazura per il logo ITASTEM. Click here and vote for @davinci.witness
This post has been voted on by the SteemSTEM curation team and voting trail in collaboration with @utopian-io.
If you appreciate the work we are doing then consider voting both projects for witness by selecting stem.witness and utopian-io!
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
better use bone cells and no more
Thanks for this useful insight, I think I'v read once some papers on oncogenic issue of this kind of therapies when used on patients with hidden bone metastasis...not everything that shines is gold
That true, also most biologics never act on their own but they often need antagonists and other biomolecules that complement their action, that's why we don't see magic pills..
I wonder how many patients have been told about this when the procedure is recommended. It may be the case, as you suggest, that few alternatives exist, but still, a patient has a right to know going in what the downside of a procedure is.
I think even the surgeons are not fully aware of the side effects of BMP-2 because they are often overlooked in scientific literature
More of something does not necessarily mean better results. Great post! Will follow.
It is important to be aware of all data and to follow subsequent research in all new products. There are plenty of examples of drugs taken off the market or with blackbox warnings added to them.
Hi @aboutcoolscience!
Your post was upvoted by Utopian.io in cooperation with @steemstem - supporting knowledge, innovation and technological advancement on the Steem Blockchain.
Contribute to Open Source with utopian.io
Learn how to contribute on our website and join the new open source economy.
Want to chat? Join the Utopian Community on Discord https://discord.gg/h52nFrV
Hi @aboutcoolscience!
Your post was upvoted by @steem-ua, new Steem dApp, using UserAuthority for algorithmic post curation!
Your UA account score is currently 4.396 which ranks you at #2182 across all Steem accounts.
Your rank has dropped 175 places in the last three days (old rank 2007).
In our last Algorithmic Curation Round, consisting of 253 contributions, your post is ranked at #197.
Evaluation of your UA score:
Feel free to join our @steem-ua Discord server