USA TODAY Investigation: VA knowingly hires doctors with past malpractice claims, discipline for poor care 2017.

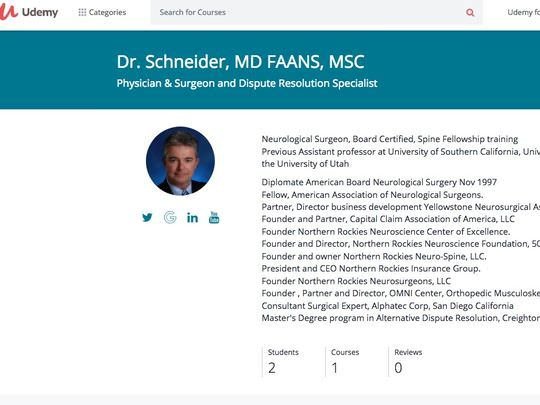
A USA TODAY investigation finds the Department of Veterans Affairs has repeatedly hired healthcare workers with problem pasts, like neurosurgeon John Henry Schneider, whose license had been revoked after a patient death. USA TODAY
Neurosurgeon John Henry Schneider racked up more than a dozen malpractice claims and settlements in two states, including cases alleging he made surgical mistakes that left patients maimed, paralyzed or dead.
He was accused of costing one patient bladder and bowel control after placing spinal screws incorrectly, he allegedly left another paralyzed from the waist down after placing a device improperly in his spinal canal. The state of Wyoming revoked his medical license after another surgical patient died.
Schneider then applied for a job earlier this year at the Department of Veterans Affairs hospital in Iowa City, Iowa. He was forthright in his application about the license revocation and other malpractice troubles.
But the VA hired him anyway.
He started work in April at a hospital that serves 184,000 veterans in 50 counties in Iowa, Illinois and Missouri.
Some of his patients already have suffered complications. Schneider performed four brain surgeries in a span of four weeks on one 65-year-old veteran who died in August, according to interviews with Schneider and family members. He has performed three spine surgeries on a 77-year-old Army veteran since July — the last two to try and clean up a lumbar infection from the first, the patient said.
Schneider’s hiring is not an isolated case.
A VA hospital in Oklahoma knowingly hired a psychiatrist previously sanctioned for sexual misconduct who went on to sleep with a VA patient, according to internal documents. A Louisiana VA clinic hired a psychologist with felony convictions. The VA ended up firing him after they determined he was a “direct threat to others” and the VA’s mission.
As a result of USA TODAY’s investigation of Schneider, VA officials determined his hiring — and potentially that of an unknown number of other doctors — was illegal.

Federal law bars the agency from hiring physicians whose license has been revoked by a state board, even if they still hold an active license in another state. Schneider still has a license in Montana, even though his Wyoming license was revoked.
VA spokesman Curt Cashour said agency officials provided hospital officials in Iowa City with “incorrect guidance” green-lighting Schneider’s hire. The VA moved to fire Schneider last Wednesday. He resigned instead.
Cashour also said the VA would look into whether other doctors had been improperly hired.
“We will take the same prompt removal action with any other improper hires we discover,” he said.
A USA TODAY investigation in October revealed how the VA has for years concealed shoddy care and mistakes by medical workers when they leave the agency, allowing them to escape their pasts and potentially endanger patients elsewhere.
The results of the investigation of Schneider and other VA practitioners with problem pasts reveal potentially dangerous shortfalls when they join the agency as well.
More: VA conceals shoddy care and health workers' mistakes
More: Exclusive: Botched surgery, delayed diagnosis at a one-star 'house of horrors' VA hospital
In response to the findings, Cashour said the agency is also initiating an “independent, third-party clinical review” of the care Schneider provided with complications in Iowa City relayed to USA TODAY by patients or family members.
In an interview, Schneider maintained that he has not provided substandard care. He blamed poor outcomes for patients on other providers involved in their treatment or on unfortunate complications not caused by his care.
Schneider said his insurance company decided to settle some of his prior cases regardless of their merit, and he filed an appeal of the Wyoming revocation, a case that's still pending.
"I'm a neurosurgeon; neurosurgeons across the country get litigation because of complications related to surgery," he said.
Of 15 malpractice complaints identified by USA TODAY, four were settled, and two were dropped by plaintiffs. Six others were deemed valid by a trustee after Schneider filed bankruptcy in 2014, court records show. The trustee rejected the other claims.
More: VA still in critical condition, Secretary David Shulkin says
More: Lawmakers rip VA on failure to report potentially dangerous medical providers
One malpractice lawyer and neurosurgeon who is not familiar with Schneider’s case said that in general, having a dozen malpractice claims in as many years raises red flags.
“That’s certainly not usual. It’s definitely an outlier.” said Larry Schlachter, author of Malpractice: A Neurosurgeon Reveals How Our Health Care System Puts Patients at Risk.
For Schneider’s former patients and their family members, news of his hiring at the VA and return to the operating room after his Wyoming license was revoked came as a shock.
“What in the world?” said Scherry Lee, who is awaiting payment for a malpractice complaint against Schneider after a failed neck surgery in Wyoming in 2012. She says it left her in debilitating pain with difficulty speaking and swallowing. “How does this happen, especially with a neurosurgeon?”
A trail of malpractice claims
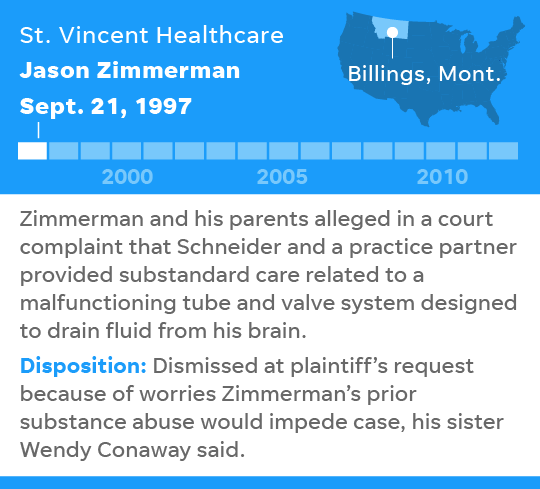
Less than two months after Montana issued Schneider a medical license in 1997, Jason Zimmerman was rushed to the emergency room at St. Vincent Healthcare in Billings.
He had excess fluid building up around his brain that was creating dangerous intracranial pressure, according to court records. A tube and valve system that had been implanted to drain excess cerebrospinal fluid had malfunctioned.
His family sued Schneider and a practice partner alleging they provided substandard care and Zimmerman suffered “profound neurological injury” that left him permanently impaired, the complaint says.
He and his family members ultimately dropped their malpractice suit because they worried Zimmerman’s prior substance abuse would impede the case, his sister Wendy Conaway told USA TODAY. Schneider blamed his partner for the injuries.
But it was only the first of four malpractice claims he would face over the next five years from surgical patients at St. Vincent hospital. The others settled for undisclosed amounts, court records show.
They included the case of Lloyd Hickey, who was paralyzed from the waist down after Schneider allegedly implanted a device improperly in his spinal canal, and Carmen Riddle, who lost bladder and bowel control after three spine surgeries by Schneider. The wife of Thomas Deiling settled her wrongful death claim against Schneider after her husband died from complications after four surgeries.
“I continued the lawsuit hoping I could force him out of practice, but I couldn’t because of the cap on medical negligence lawsuits,” Jeanine Deiling said in a recent interview. She said Schneider failed to properly diagnose and quickly treat a pervasive infection that ended up eating away at her husband's spine.
Her best hope, Deiling said, was to add hers to the list of malpractice claims, and “if enough lawsuits added up, he’d never be able to get malpractice insurance and he’d have to quit practicing.”
Schneider did stop performing surgeries in Montana, but he started performing them in Wyoming instead. And he formed a company, Northern Rockies Insurance Company, that provided his own malpractice insurance, a move that eventually helped land him in bankruptcy and unable to pay off all his claims.
At hospitals in Cody and Powell, Wyo., and a surgical center in Sheridan, Wyo., Schneider performed operations between 2006 and 2012 that eventually prompted at least eight more malpractice complaints.
The case that captured the attention of Wyoming Board of Medicine officials was Russell Monaco, a father of two who went under Schneider’s knife in 2011 for a procedure to decrease pressure on nerves in his lower back, according to a wrongful death suit filed by his wife, Kathy.
After the operation, he was prescribed a litany of narcotics that can depress breathing, including fentanyl, oxycodone, valium, and Demerol. Monaco’s oxygen levels dropped dangerously low, but Schneider discharged him anyway, medical board records show.
He went home and took the medications as prescribed, the lawsuit says, but his family found him dead the next morning. The coroner determined the cause of death was “mixed drug overdose.”
“I tried to wake him up and yelled and the girls came down screaming,” his wife, Kathy Monaco, told USA TODAY. “It was horrible, I mean, I live that day over every day.”
The Wyoming Board swiftly placed restrictions on Schneider’s license and ultimately revoked it in 2014.
Schneider filed bankruptcy in December that year, leaving malpractice claimants hanging without payment even now, including the Monaco family.
In an interview, Schneider laid blame for Monaco's death on a physician assistant who prescribed the medications. He said an aide in the operating room caused Hickey's paralysis, and he blamed Riddle's injury on a hematoma caused by medications prescribed by another provider. In Deiling's case, Schneider asserted standard tests didn't initially pick up the infection or indicate he needed more timely treatment.
Vetting revelations
The VA hiring process is seemingly rigorous.
Applications are vetted, education and licenses verified, references checked, and interviews conducted. For clinical hires, a review and approval by a professional standards board also is required.
But when applicants disclose prior problems with medical licensing short of revocation, malpractice or criminal histories, VA hospital officials have discretion to weigh the providers’ explanations and approve their hiring anyway.
The VA hospital in Muskogee, Okla., hired a psychiatrist in 2013 with multiple disciplinary actions against his Oklahoma license, including for sexual misconduct, according to internal documents obtained by USA TODAY.
Hospital officials knew about his past, but approved his hiring anyway with the condition he be closely monitored during his probation period, the documents show.
And yet the psychiatrist, Stephen Lester Greer, went on to have a sexual relationship with a VA patient and ended up pleading guilty in August to witness tampering for trying to persuade the patient to lie about it to federal investigators.
More: Candid Veterans Affairs nominee faces big challenges to fix entrenched bureaucracy
More: VA vows changes on bad health care providers, lawmakers take action after USA TODAY investigation
The VA hired a psychologist to work at a clinic in Lafayette, La., in 2004, despite his revealing previous felony convictions on his application, according to the internal documents, which don’t identify the provider by name. The VA didn’t run a criminal background check until a year after he started work. It showed eight arrests, including for burglary, drug dealing and reckless driving resulting in death.
Still the VA allowed him to continue practicing until two years ago. By that time, the VA had received multiple complaints about patient mistreatment by the psychologist. An internal investigation found he was a “direct threat to others, (and) to the Department’s mission.” The VA fired him earlier this year.
The VA hospital in Jackson, Miss., hired ophthalmologist Daniel K. Kim, despite his being sanctioned by licensing authorities in Georgia. During his subsequent surgeries at the VA, a World War II veteran was blinded in 2006 and he allegedly implanted the wrong lens in another patient’s eye in 2012. Kim has denied any wrongdoing, and a VA investigation suggested a nurse assisting Kim caused the blinding.
More: Veteran patients in imminent danger at VA hospital in D.C., investigation finds
More: Senators author bill forcing VA to report more problem medical providers, faster
Psychiatrist David Houlihan landed a job at a VA hospital in Wisconsin in 2002 and was promoted to chief of staff two years later, even though the Iowa Board of Medicine had charged him with engaging in an inappropriate relationship with a patient and taking patient medications home.
He went on to earn the nickname “candy man” at the Tomah, Wis., VA because of the prolific amounts of narcotics he prescribed. The VA fired Houlihan in 2015 after revelations a 35-year-old veteran patient had died from mixed drug toxicity at the facility. He has denied any wrongdoing, but agreed to surrender his medical license in Wisconsin earlier this year.
Some of the VA’s policies can attract medical workers with past malpractice or licensing problems. Agency clinicians aren’t required to have malpractice insurance — the federal government pays out claims using taxpayer dollars — making the VA a good fit for providers who may have difficulties securing malpractice insurance in the private sector if past issues have rendered them too risky.
The Iowa City VA had been looking for a full-time neurosurgeon for nearly a year when Schneider came along.
In his job application, Schneider disclosed “all the issues” and the VA hired him after a “group of his medical peers thoroughly reviewed” his file and “approved his competency,” the VA said in a prepared statement provided to USA TODAY.
Schneider began work in April at an annual salary of $385,000.
Complicated surgeries
Complications soon began cropping up.
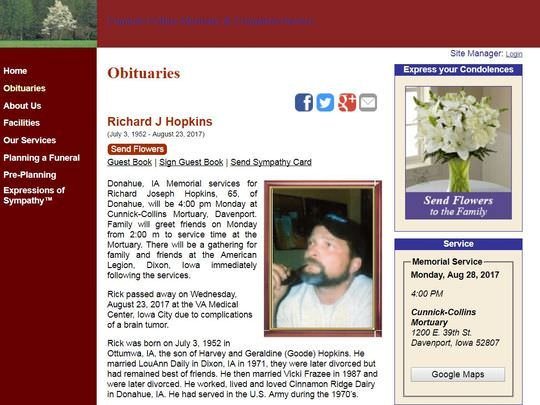
Schneider, who describes himself as a spinal specialist, performed surgery in July to remove a benign tumor from a 65-year-old patient's brain.
Richard Joseph Hopkins survived three more brain surgeries for ensuing complications before dying Aug. 23 from infection.
“Rick was strong, he was a bull,” his sister Annette Rainsford said. “Why would you go into someone’s head four times?”

James Wehmeyer, a 77-year-old Army veteran, said Schneider performed his first spinal procedure in July. The neurosurgeon subsequently did two more operations to try and clean up infection from the first, prompting concerns something might be amiss with his treatment.
“I thought that, but I didn’t know,” he said. “I’m not a doctor.”
Wehmeyer said it’s been a month since his last surgery, and a nurse still visits him at home every three days to clean out the wound, which he said hasn’t healed.
“There’s a big hole in there they’re trying to close up,” he said.
At least three other patients suffered infections after procedures Schneider conducted at the Iowa City VA — two deep-wound and one superficial — but they were cured with antibiotics, Schneider said.
In September, Schneider was arrested on federal criminal charges of lying and trying to conceal assets in his bankruptcy case in Montana.
His patients in Iowa City showed up for surgery but had to be rescheduled when he didn’t show up for work. Schneider told his VA bosses what happened when he got back to Iowa.
He continued practicing.
Schneider, who pleaded not guilty to the charges, said in an interview that infections suffered by his VA patients were not his fault, but rather complications that can occur in neurosurgery.
He said Hopkins' case was a "tragic" example, where he developed two brain bleeds and then fluid buildup, each requiring another surgery.
"I've had a great run at the VA with zero issues," he said. "Have I had to take patients back (for surgery) for post-op infection? Yes. I mean, I can't prevent every infection."
One of Schneider’s patients from Wyoming said that whatever the case, the VA never should have hired him.
“Here the veterans, they went and served their country, and they’re messed up and everything,” said Michael Green, who is awaiting payment for a malpractice claim that alleged Schneider placed a screw incorrectly in his lower spine. “And then turn that guy loose on them, that’s what doesn’t make sense.
Sorch:https://www.usatoday.com/story/news/politics/2017/12/03/usa-today-investigation-va-knowingly-hires-doctors-past-malpractice-claims-discipline-poor-care/909170001/