8 fascinating facts about heartburnBothered by heartburn? We share a few interesting facts.Heartburn: 9 FAQs 7 ways coughing can injure your body

Heartburn is a cause of pain and discomfort in millions of people. ~
If you can’t look at a hamburger without getting a burning sensation in your chest and a bitter taste in your mouth, you’re not alone. Heartburn is one of the world’s most common ailments.
But how much do you really know about it? Have a look at these surprising facts – you may learn a thing or two that will douse the flames...
About 25% of the sensory fibres connecting your oesophagus to your brain pass close to neurons that also receive sensory information from your heart. This is why it’s sometimes difficult to distinguish pain related to a problem with the heart (e.g. angina) from pain in the oesophagus (e.g. heartburn).
Chewing bubble gum may not always be socially acceptable, but it can help to relieve heartburn. Chewing on something increases the production of saliva, which helps to neutralise stomach acid.
Nocturnal gastro-oesophageal reflux disease (GORD) leads to reflux and heartburn while one sleeps, and is a fairly common occurrance. But did you know that nocturnal GORD can increase your risk for inflammation of the lining of the nose? If you experience a stuffy or runny nose, and often sneeze in the absence of a cold, you may have nocturnal GORD.
Sleeping on extra pillows won’t necessarily help to alleviate heartburn when you sleep or lie down, as you may slip down in the night. Elevate your bed by about 15cm instead (place bricks or blocks under the feet). Gravity will work in your favour and less acid will flow back up into your oesophagus.
Some people with GORD experience changes in taste and smell, which could affect their enjoyment of food. Acid reflux may cause damage to the palate and has the potential to cause taste abnormalities – another reason why it’s important to get heartburn checked out by a doctor.
Apart from negatively affecting the functioning of your lower oesophageal sphincter (the valve-like structure between the oesophagus and stomach), smoking can also affect your heartburn medication (e.g. cimitidine). Smoking impairs the ability of the medication to lower the production of stomach acid while you sleep.
While it’s best to avoid acidic foods like tomatoes, berries and citrus fruits when your oesophagus is inflamed as the acid may cause irritation, these foods have little effect on the pH of your stomach. Gastric juice has a pH of 2.0, while lemon juice has a pH closer to 2.5/3.0. So, eating acidic foods can't cause the stomach to become more acidic – it’s already as acidic as it can be.
Chronic obstructive pulmonary disease (COPD), which includes emphysema and chronic bronchitis, is closely linked to GORD. Research shows that over 50% of people with later stages of COPD also have GORD. COPD may lead to frequent increases in intra-abdominal pressure, which contribute to reflux and heartburn. In turn, the reflux associated with GORD can increase COPD symptoms (e.g. coughing and wheezing), and trigger flare-ups.
Reference:
- Mahan, LK. Escott-Stump, S. Raymond, JL. (2012) Krause’s Food and the Nutrition Care Process - 13thedition. Elsevier. ISBN: 978-1-4377-2233-8
Image credit: iStock
Carine Visagie
http://www.health24.com/Medical/Heartburn/News/8-fascinating-facts-about-heartburn-20171024#cxrecs_s
Do you often feel like your chest is on fire after eating? If you do, you probably suffer from heartburn. We answer some important questions about this common ailment.
0
There are many questions about how best to treat heartburn. ~
- Can I take OTC antacids and prescription meds together?
If you suffer from heartburn, indigestion, a peptic ulcer and/or gastro-oesophageal reflux disease (GORD), your doctor may prescribe a proton pump inhibitor such as lansoprazole or omeprazole, or an H2 receptor antagonist like ranitidine or cimetidine.
While you can still take antacids with these medicines (especially during the first few days before your prescription medicine starts working), it’s best not to take them at the exact same time. Don’t take an antacid within an hour before or after taking an H2 blocker or proton pump inhibitor.
Both proton pump inhibitors and H2 receptor antagonists reduce the amount of acid produced in the stomach. If you take an antacid with your prescription medicine, it may affect absorption and make the medicine less effective.
The pH in the stomach needs to be low enough for the proton pump inhibitor or H2 receptor antagonist to work. The acid activates the medicine. Also talk to your doctor about any other possible drug interactions.
Some of your other medications, supplements and/or herbal remedies may also interact with your prescription medicine for heartburn. Always carefully read the package insert before you start taking new medication.
- I have a medical condition. Is it safe to take OTC antacids?
This will depend on your medical condition and the kind of antacid you’re planning to take, but if you have kidney disease, liver disease, hypertension, heart failure, haemorrhoids, gastrointestinal blockages, or chronic constipation or diarrhoea, it’s best to first check with your doctor.
Here are a few examples of what can go wrong if you take antacids:
If you have renal failure, long-term use of antacids that contain aluminium hydroxide may result in an increased concentration of aluminium in your blood. This, in turn, is linked to dialysis encephalopathy (where the functioning of the brain is affected) and dialysis osteomalacia (softening of the bones). Overuse of antacids that contain calcium carbonate, on the other hand, may lead to milk-alkali syndrome, where blood levels of calcium are too high and calcium is deposited in the kidneys – another dangerous situation.
If you need to control the amount of salt you eat – for example because you have hypertension, renal failure, oedema or cirrhosis of the liver – it’s also best to steer clear of certain antacids. When “sodium” is listed as one of the ingredients (e.g. sodium bicarbonate), the antacid may contain high levels of salt.
Magnesium-containing antacids can act as laxatives. If you already suffer from diarrhoea, these antacids may contribute to even greater fluid and electrolyte losses, so it’s best to steer clear of these.
Other kinds of antacids can lead to constipation. If you find that your current antacid makes you constipated, opt for a magnesium hydroxide or aluminium hydroxide antacid instead.
If you’re in good health, antacids are generally safe to take as directed. But if you have an existing medical condition (even if it’s not one of the conditions mentioned above), it’s important to talk to your doctor before taking an antacid. Also read the package insert carefully to check for contraindications and possible side effects.
- Can stress make heartburn worse?
Although there 's no clear link between stress and heartburn, it is known that some people become more aware of symptoms of heartburn and other symptoms of gastro-oesophageal reflux disease (GORD) when they’re feeling stressed and anxious. This is especially true in people who have been exposed to prolonged life stressors.
Mental disorders also often overlap with gastrointestinal symptoms, of which heartburn may be one.
In a 2015 study published in Przeglad Gastroenterologiczny, for example, researchers analysed whether abdominal symptoms such as heartburn and stressful situations overlapped, as reported by patients who were being treated with psychotherapy. In many instances, symptoms of anxiety disorders coexisted with irritable bowel syndrome (IBS) and functional dyspepsia – a chronic condition that causes pain or discomfort in the upper gastrointestinal tract.
- Why do I get heartburn when I lie down?
The mechanism is simple: lying flat means it’s easier for stomach acid to move upwards (or “reflux”) into your oesophagus, from where it can cause the pain and discomfort associated with heartburn.
Research shows that night-time heartburn occurs in more than 70% of adults with gastro-oesophageal reflux disease (GORD). This can lead to sleeping problems and a reduced quality of life. In turn, sleep deprivation can enhance the perception of acid in the oesophagus.
Night-time reflux tends to be more damaging to the oesophagus than reflux experienced during the day, and has been linked to a higher risk of inflammation, Barrett’s oesophagus and oesophageal cancer.
It may help to elevate the head of your bed. Simply put the top section of your bed on bricks or blocks, or sleep on a wedge-shaped pillow. Gravity will help clear the refluxed stomach contents from your oesophagus.
Also try to lose weight if you’re overweight or obese, as this may contribute to heartburn. And talk to your doctor – prescription medication in the form of a proton pump inhibitor or H2 receptor antagonist may make a world of difference.
- Can heartburn cause cancer?
If you frequently suffer from heartburn, chances are that you have gastro-oesophageal reflux disease (GORD). Unfortunately, this also means you have a higher risk for cancer of the oesophagus. The more frequent your symptoms, the greater the risk.
When you experience heartburn regularly, the cells in the lining of your oesophagus may start to change – so much so that they start to look like the tissue found in the small intestine. This is called Barrett’s oesophagus, a condition that sometimes develops into cancer.
If you are ever diagnosed with Barrett’s oesophagus, your doctor will monitor you closely over time to check for cancer. If cancer develops, you might have to undergo surgery.
Apart from cancer of the oesophagus, heartburn is also associated with cancer of the throat and vocal cord. Interestingly, research shows that taking a simple over-the-counter antacid may lower your risk.
Remember: it’s not normal to experience heartburn several times a week. Talk to your doctor if this is the case.
- I have heartburn. Will it help to drink a glass of milk?
While milk can provide a temporary buffer to stomach acid, it’s best not to use this beverage as a way to manage frequent heartburn. There are two reasons why:
Milk is rich in calcium and too much calcium in the diet may lead to milk-alkali syndrome. When this occurs, blood levels of calcium are too high and the mineral is deposited in the kidneys – a dangerous situation that can lead to renal failure.
Milk may lead to increased acid production in the stomach, which may make heartburn worse. The calcium, fat and protein in milk are all stimulants for stomach-acid production, research conducted as far back as 1976 showed.
But if you’re really stuck, and don’t have an antacid on hand, a small glass of fat-free or low-fat milk may provide temporary relief.
- Can certain medicines cause heartburn?
Yes, some medicines can indeed cause heartburn. These include:
Tablets for motion sickness (anticholinergics)
Beta blockers (also known as beta-adrenergic blocking agents), used to reduce blood pressure
Calcium-channel blockers (also known as calcium-channel antagonists), used to relax blood vessels
Dopamine-like drugs, used to treat Parkinson’s disease
Progestin, a synthetic form of progesterone used in oral contraceptives and hormone replacement therapy (HRT)
Sedatives
Theophylline, used for treating respiratory diseases like chronic obstructive pulmonary disease (COPD) and asthma
Tricyclic antidepressants, used to treat depression
If you believe one of your medications could be causing your heartburn, it’s important not to stop taking your medication before checking with your doctor.
- Are asthma and heartburn related?
It’s estimated that more than 75% of people with asthma also experience gastro-oesophageal reflux disease (GORD). GORD may be a trigger for asthma, and asthma may trigger reflux and heartburn.
How this link works, exactly, isn’t 100% clear yet. One underlying reason for the connection could be aspiration, where refluxed stomach contents enter the lung directly via the mouth, causing irritation and, subsequently, asthma symptoms. Another theory is that refluxed stomach acid irritates the nerve endings in the oesophagus. A signal is then sent to the brain, and the brain responds by telling the airways to produce mucus. This may lead to constriction of the airways and asthma.
Your doctor might suspect GORD if your asthma symptoms don’t respond well to treatment, or if your asthma becomes worse when you exercise or after you’ve eaten a meal.
Although a Cochrane review found that using medication for reflux doesn’t generally help ease asthma symptoms, some people do benefit. Discuss your symptoms and treatment options with your doctor.
- Why does stomach acid burn my oesophagus, but not my stomach?
The hydrochloric acid in your stomach is incredibly acidic – so much so that it’s been likened to battery acid. It needs to be this acidic to destroy germs and to help with the digestion of food.
But while hydrochloric acid can be incredibly damaging to your oesophagus, teeth and even your upper respiratory tract, your stomach copes with it just fine. Well, most of the time, anyway.
The acid present in your stomach doesn’t digest the stomach lining for several reasons. One is that the specialised cells in the stomach’s mucosa (the mucous membrane that lines the inside of the stomach) secrete large quantities of protective mucus and bicarbonate – both of which coat the lining of the stomach and keep the acid from causing harm. But the system has its flaws. A bacterium called Helicobacter pylori thrives in the acidic environment of the stomach. An infection with this bacteria can lead to lesions in the lining of the stomach, which may cause stomach ulcers.
Image credit: iStock
Carine Visagie
http://www.health24.com/Medical/Heartburn/News/heartburn-9-faqs-20171027#cxrecs_s
The average cough lasts between two and three weeks and usually causes no serious physical damage – but beware when a cough turns violent!
0
Violent coughing can cause physical damage. ~
A cough is the rapid expulsion of air from the lungs to clear the throat and airways of mucus, foreign particles, fluids, microbes and various irritants.
A 2013 review found that the average cough lasts around 18 days. After more than eight weeks, a cough can be regarded as chronic and it is advisable to seek medical advice.
According to a previous Health24 article, many people let a persistent cough go untreated for too long. A doctor can help you find out if your cough is symptomatic of something more serious.
'Structural damage'
A cough can sometimes affect your health in unexpected ways. Apart from indicating illnesses like TB and some cancers, a chronic cough can also cause social embarrassment, interfere with sleeping patterns, as well as cause headaches and urinary incontinence.
But that's not all – violent, persistent coughing can actually cause “structural” damage to your body:
- Muscular pain
Persistent coughing can lead to chronic muscular pain. Every time you have a coughing fit, strong pressure is generated, which can strain muscles and cause pain.
- Cracked ribs
Rib fractures caused by chronic coughing mainly occur in women. The middle ribs along the side are mostly affected. Lower bone density is a risk factor, but cough-induced rib fractures can also happen in people with normal bone density.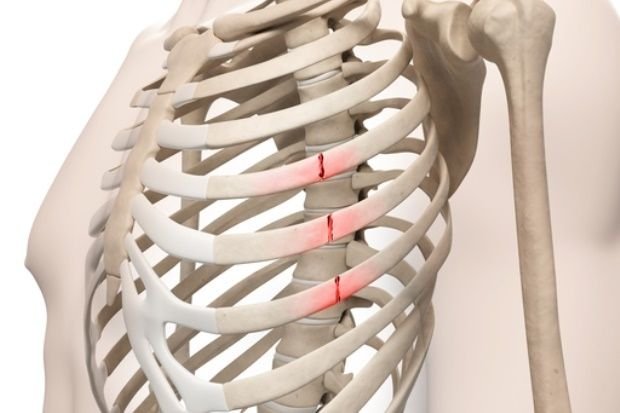
- Damage to small blood vessels
Violent coughing fits may cause fine blood vessels (in the anus and nose, for example) to burst, leading to haemorrhage. 
- Rupture of the diaphragm
The diaphragm contracts during the expiratory phase of a cough. During forced respiratory movements, the diaphragm is pushed upward while the ribs are pushed inward and downward. This opposing action can sometimes result in diaphragmatic rupture. 
- Abdominal hernia
Although damage to the abdominal wall after coughing is rare, it may require surgical intervention. Both abdominal herniations and abdominal muscle tears have been reported. Abdominal muscle tears are difficult to detect and tend to occur in patients with chronic bronchitis. However, abdominal hernias caused by cough are easier to detect.
- Tissue damage in the throat
Persistent coughing can cause throat infections, which can lead to an infection risk to other parts of the body. A chronic cough may also cause inflammation in the tissues of the throat. 
- Coughing up blood
The medical term for coughing up blood is heamoptysis. If you're coughing up small amounts of bright red blood or frothy blood-streaked saliva and phlegm, it usually indicates blood from your lungs due to prolonged coughing or a chest infection. 
Image credits: iStock
Eugene Lotter
http://www.health24.com/Medical/Cough/News/7-ways-coughing-can-injure-your-body-20170922#cxrecs_s
to get $15-$20 on a day.
https://www.bestchange.com/?p=377237
thanks