Turner Syndrome
-- DIFFERENTIAL DIAGNOSIS AND RECOMMENDED TREATMENT
EVALUATION:
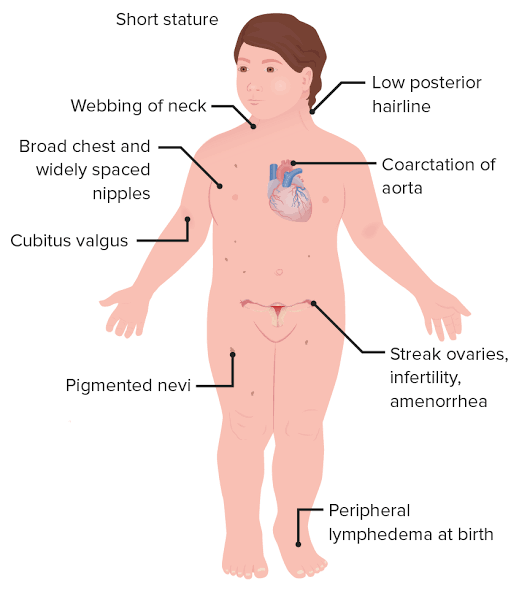
- Short stature compared to peers and family members.
- Dysmorphic features such as webbed neck, shield-like chest with widely spaced nipples, and cubitus valgus.
- Congenital lymphedema of the hands and feet, particularly in neonates.
- Primary amenorrhea and delayed puberty due to ovarian dysgenesis.
- Increased risk of cardiovascular anomalies, such as coarctation of the aorta.
- Hearing loss, hypothyroidism, and liver function abnormalities in older patients.
- Skeletal anomalies such as short fourth metacarpals and metatarsals, and scoliosis.
- Increased risk of autoimmune conditions, including hypothyroidism.
DIFFERENTIAL DIAGNOSIS
POSSIBLE ETIOLOGY #1: TURNER SYNDROME
Turner Syndrome is a genetic condition caused by the complete or partial absence of one X chromosome (45, X karyotype or mosaicism). It is characterized by short stature, dysmorphic features, and gonadal dysgenesis leading to primary amenorrhea and infertility. Other associated findings include congenital lymphedema, cardiovascular anomalies, and autoimmune thyroid disease.
Diagnostic Tests: - Karyotype Analysis: To confirm the diagnosis by identifying the 45, X karyotype or mosaicism (e.g., 45, X/46, XX or 45, X/46, XY). This is the gold standard for diagnosis.
- Echocardiogram: To evaluate for congenital heart defects such as coarctation of the aorta or bicuspid aortic valve.
- Thyroid Function Tests: To assess for hypothyroidism, which is common in Turner Syndrome.
- Liver Function Tests: To check for mild liver enzyme elevation, which may improve with hormone therapy.
- Bone Age X-ray: To assess growth potential and skeletal maturity.
- Hearing Tests: To evaluate for hearing loss, which is common in Turner Syndrome.
- Pelvic Ultrasound: To assess ovarian dysgenesis and uterine development.
Recommended Treatment/Medicines: - Recombinant Human Growth Hormone (Somatropin): To address short stature. Dosage: 0.045–0.05 mg/kg/day subcutaneously. Monitor for side effects such as scoliosis progression and glucose intolerance.
- Estrogen Replacement Therapy: Begin at around 12 years of age with low-dose estradiol (e.g., transdermal estradiol 0.2–0.4 mg every 4 weeks) and gradually increase to adult doses over 2–4 years. Add cyclic progesterone after 2 years of estrogen therapy or when breakthrough bleeding occurs.
- Cardiovascular Monitoring and Management: Regular follow-up with a cardiologist for congenital heart defects. Surgical intervention may be required for severe coarctation of the aorta.
- Thyroid Hormone Replacement: If hypothyroidism is diagnosed, initiate levothyroxine therapy with regular monitoring of TSH and free T4 levels.
- Psychosocial Support: Counseling and support groups to address psychosocial challenges related to infertility and body image.
POSSIBLE ETIOLOGY #2: NOONAN SYNDROME
Noonan Syndrome is an autosomal dominant disorder that shares some overlapping features with Turner Syndrome, such as short stature, webbed neck, and congenital heart defects. However, it affects both males and females and is associated with proportionate short stature and facial dysmorphism (e.g., hypertelorism, downward slanting eyes).
Diagnostic Tests: - Genetic Testing: To identify mutations in genes associated with Noonan Syndrome (e.g., PTPN11, SOS1).
- Echocardiogram: To evaluate for pulmonary valve stenosis or hypertrophic cardiomyopathy, which are common in Noonan Syndrome.
- Growth Hormone Stimulation Test: To assess for growth hormone deficiency if short stature is present.
- Hearing Tests: To evaluate for hearing loss, which may occur in Noonan Syndrome.
Recommended Treatment/Medicines: - Recombinant Human Growth Hormone (Somatropin): For short stature if growth hormone deficiency is confirmed. Dosage: 0.045–0.05 mg/kg/day subcutaneously.
- Cardiovascular Monitoring and Management: Regular follow-up with a cardiologist for congenital heart defects. Surgical intervention may be required for severe cases.
- Educational and Developmental Support: Early intervention programs for developmental delays and learning disabilities.
PRECAUTIONS - Avoid high doses of growth hormone in patients with scoliosis, as rapid growth may worsen the condition.
- Monitor for signs of glucose intolerance or diabetes during growth hormone therapy.
- Avoid estrogen therapy in patients with a history of thromboembolic events or uncontrolled hypertension.
- Regularly monitor cardiovascular status to prevent complications such as aortic dissection or hypertension.
FOLLOW-UP CLINICAL QUESTIONS - Are there any family members with similar symptoms or a history of genetic disorders?
- Has the patient experienced recurrent ear infections or hearing loss?
- Are there any signs of delayed puberty or menstrual irregularities?
- Has the patient undergone any previous genetic testing or imaging studies?
- Are there any symptoms of hypothyroidism, such as fatigue, weight gain, or cold intolerance?
-- PATIENT EDUCATION
PRECAUTIONS AT HOME: - Monitor for any signs of swelling (lymphedema) in the hands, feet, or neck, especially in infants. If swelling is noticed, consult a healthcare provider promptly.
- Ensure regular cardiovascular check-ups, as Turner syndrome is associated with heart defects such as coarctation of the aorta. Avoid activities that may strain the heart without prior medical clearance.
- Be vigilant about developmental milestones, as children with Turner syndrome may have an increased risk of developmental issues, such as hip dysplasia. Early intervention can help address these concerns.
- Maintain a healthy and balanced diet to support growth and development. Children with Turner syndrome may have specific dietary needs, so consult a dietitian if necessary.
- Encourage physical activity appropriate for the child’s age and abilities, but avoid high-impact activities if there are concerns about joint or bone health.
FURTHER STEPS AND CONSULTS: - Schedule a genetic test if Turner syndrome is suspected. This blood test can confirm the diagnosis by identifying the chromosomal abnormality.
- Work closely with a pediatric endocrinologist to monitor and manage growth and hormonal development. Growth hormone therapy may be recommended to address short stature, a common feature of Turner syndrome.
- Consult a cardiologist to evaluate and monitor heart health, as heart defects are common in Turner syndrome.
- If developmental delays or learning difficulties are observed, seek support from a developmental pediatrician or educational specialist. Early intervention programs can be beneficial.
- Consider seeing an orthopedic specialist if there are concerns about hip dysplasia or other skeletal abnormalities.
OTHER CONSIDERATIONS - Be aware that Turner syndrome can lead to primary ovarian insufficiency, which may affect fertility and hormone levels. Discuss long-term reproductive health with a healthcare provider as the child approaches adolescence.
- Emotional and psychological support is important. Children with Turner syndrome may face challenges related to self-esteem or social interactions due to physical differences. Counseling or support groups can be helpful.
- Regular vision and hearing screenings are recommended, as Turner syndrome can sometimes be associated with issues in these areas.
- Educate family members and caregivers about the condition to ensure a supportive environment for the child.
- Keep a detailed medical history and share it with all healthcare providers to ensure coordinated care across specialties.
Recommended Readings
Oxford Textbook of Medicine
https://www.drugs.com/cg/failure-to-thrive.html
https://www.drugs.com/health-guide/tourette-syndrome.html
https://www.drugs.com/mtm/genotropin.html
https://www.drugs.com/ppa/somatropin.html
https://www.merckmanuals.com/home/children-s-health-issues/chromosome-and-gene-abnormalities/turner-syndrome
https://www.merckmanuals.com/professional/pediatrics/chromosome-and-gene-anomalies/turner-syndrome
https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-turner-syndrome
https://www.uptodate.com/contents/cutis-verticis-gyrata
https://www.uptodate.com/contents/estradiol-systemic-drug-information
https://www.uptodate.com/contents/primary-ovarian-insufficiency-beyond-the-basics
https://www.uptodate.com/contents/recombinant-human-growth-hormone-somatropin-drug-information
https://www.uptodate.com/contents/recombinant-human-growth-hormone-somatropin-pediatric-drug-information
https://www.uptodate.com/contents/sex-chromosome-abnormalities
https://www.uptodate.com/contents/tourette-syndrome-the-basics
https://www.uptodate.com/contents/turner-syndrome-the-basics