SEC S20W1 || Hematopoiesis - Module 1
Assalam-o-Alaikum!!!
Edit in poster my Wall
Greetings to my all STEEMIT members. hopefully, you all are fine and enjoying your best life on STEEMIT. Today I will share my post that I am going to participate in this homework task. And I am sure that I will share quality content and I will answer the all questions
Hematopoietic organs are responsible for the production, maturation and regulation of blood cells, which are important for oxygen transport, immune defense and other vital functions.. Each organ plays a specific role in hematopoiesis (formation of blood cells) and maintenance of the immune system.
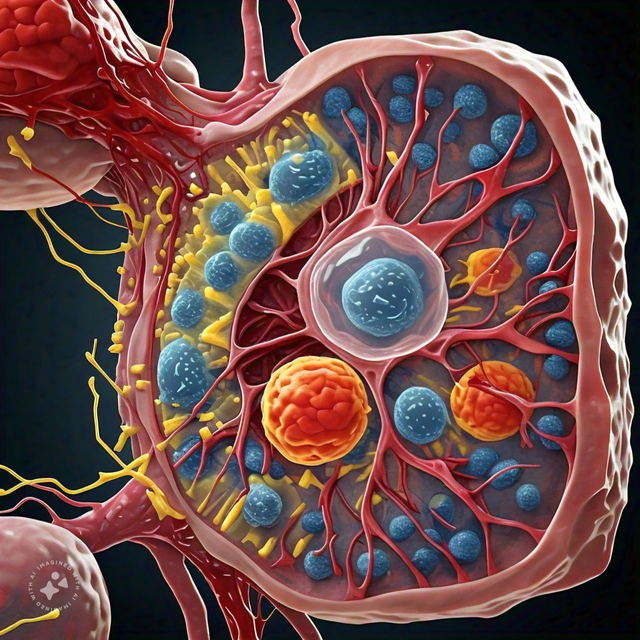
1. Bone marrow
Anatomy: Located within the cavities of bones, especially long bones (such as the femur and humerus), pelvis, sternum, and vertebrae.
- Function:
Primary site of hematopoiesis in adults.It Contains hematopoietic stem cells which differentiate into all types of blood cells: red blood cells , white blood cells (WBCs), and platelets.
The red pulp is active in the production of blood cells, while the yolk marrow (mainly fat) can return to active hematopoiesis if needed.
Blood cell production is regulated by growth factors such as erythropoietin, thrombopoietin, and colony stimulating factors (CSFs).
2. Spleen
Anatomy: Located in the upper left quadrant of the abdomen, just below the diaphragm.
- Function:
Acts as a blood filter, removing old or damaged RBCs. Stores WBCs, especially lymphocytes and monocytes, and releases them during immune responses.
In the white pulp, it facilitates immune function, generates lymphocytes and activates the immune response. It also acts as a reservoir for platelets and helps recycle iron from RBC breakdown.
3. Thomas
Anatomy: A small, bilobed organ located in the upper back of the chest, behind the sternum.
- Function:
Essential for the maturation of T-lymphocytes (T cells), a type of WBC important for adaptive immunity. Thymocytes (immature T cells) from the bone marrow migrate to the thymus, where they undergo maturation and selection to become activated T cells capable of recognizing pathogens without attacking the body's own tissues. The thymus is most active in childhood and slows down (shrinks) in adulthood.
4. Lymph nodes
Anatomy: Small, bean-shaped structures located throughout the body along the lymphatic system, especially in the neck, armpits, back, and abdomen.
- Function:
-Act as sites where immune cells (lymphocytes) can encounter antigens, become activated, and mount an immune response.
-Contains B-lymphocytes (B cells) and T-lymphocytes (T cells), which are essential for adaptive immunity. B cells produce antibodies, while T cells kill infected cells and regulate the immune response.
Summary of Functions:
Bone marrow: production of blood cells (RBCs, WBCs, platelets).
Spleen: Blood filtration, RBC recycling, storage of immune cells.
Thomas: T cell maturation and selection.
1. Medullary Hematopoiesis
This refers to the normal production of blood cells within the bone marrow, mainly in the red pulp of bones such as ribs, vertebrae and long bones such as the femur and humerus.
Process:
These stem cells differentiate into different types of blood cells through the process of stem cell development. This is the normal steady-state process of hematopoiesis in adults, with the bone marrow serving as a critical site for the production of healthy cells. In humans, the production of almost all blood cells is confined to the bone marrow after birth, in which the red marrow performs the function.
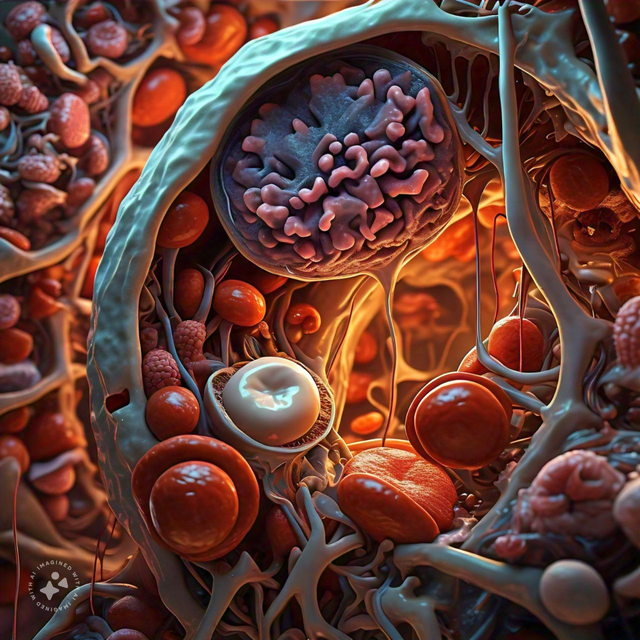
2. Extramedullary Hematopoiesis (EMH)
This refers to the formation of the blood base outside the bone marrow. Other common sites of extramedullary homeopoiesis are the liver, spleen, and sometimes other tissues, such as the adrenal glands or even the adrenal glands.
Process:
The body is present to meet the demand for blood cells due to illness or other reasons. These other charges that have hematopoietic functions during embryogenesis produce blood cells that reactivate their side. It can be a severe bleeding mechanism from myelofibrosis, a bone marrow failure
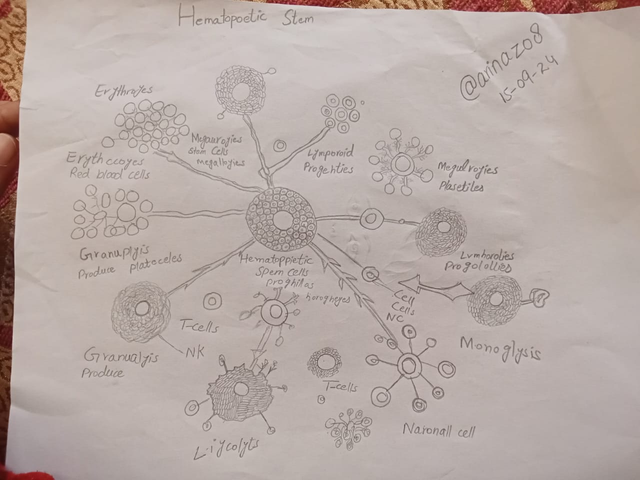
Myeloid progenitor leads to:
Megakaryocytes, which produce platelets involved in clotting.
Granulocytes such as neutrophils, basophils, and eosinophils, which are part of the immune response.
Monocytes, which become macrophages that engulf pathogens.
Lymphoid progenitors lead to:
- T cells (cell-mediated immunity).
- B cells (produce antibodies).
- These structural branches ensure the balanced production of various blood cells for immunity, oxygen transport and clotting.
Here is the screen shot of the Quiz Result
 |  |
|---|
Based on the patient's presentation and test results, the reasons for significant blood loss in this 25-year-old male patient following a car crash could be:
1. Trauma-induced injuries:
The patient has bruises all over his body, indicating multiple sites of trauma. This can lead to bleeding from damaged blood vessels, tissues, and organs
2. Broken femur:
The fractured femur (thigh bone) can cause significant blood loss due to bleeding from the bone marrow, surrounding soft tissues, and damaged blood vessels.
3. Internal injuries:
Although not explicitly stated, internal injuries such as bleeding from organs like the spleen, liver, or lungs cannot be ruled out.
4. Vascular damage:
The trauma from the car crash may have damaged blood vessels, including arteries and veins, leading to uncontrolled bleeding.
5. Soft tissue damage:
The patient's bruises suggest soft tissue damage, which can cause bleeding into the surrounding tissues.
6. Hematoma formation:
Blood accumulation at the site of injury (hematoma) can lead to significant blood loss.
7. Coagulopathy:
Trauma can disrupt the body's clotting mechanism, leading to uncontrolled bleeding.

Q:4 b)Who would be the ideal person to donate blood to? (profile of the ideal donor)
The ideal person to donate blood to the 25-year-old male patient would be someone with a compatible blood type and characteristics. Here's what I mean:
Blood Type: The donor should have the same blood type as the patient, which is not specified in the scenario. However, assuming the patient has a common blood type like Type O, A, B, or AB, the donor should match that type.
Rh Factor: The donor's Rh factor (positive or negative) should also match the patient's Rh factor.
Cross-Matching: Before transfusion, a cross-match test should be performed to ensure the donor's blood is compatible with the patient's blood.
Age and Health: The ideal donor should be between 18 and 65 years old, in good overall health, and meet specific medical criteria (e.g., no recent travel to areas with high infectious disease risk).
Blood Component: Depending on the patient's needs, the donor may be asked to donate a specific blood component, such as:
- Whole blood
- Red blood cells (RBCs)
- Plasma
- Platelets


Special Thanks to: @aaliarubab, @dexyluz
Invite Friends: @eliany, @memamun, @wakeupkitty
Upvoted. Thank You for sending some of your rewards to @null. It will make Steem stronger.