Peptic ulcer
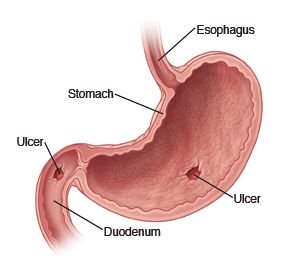
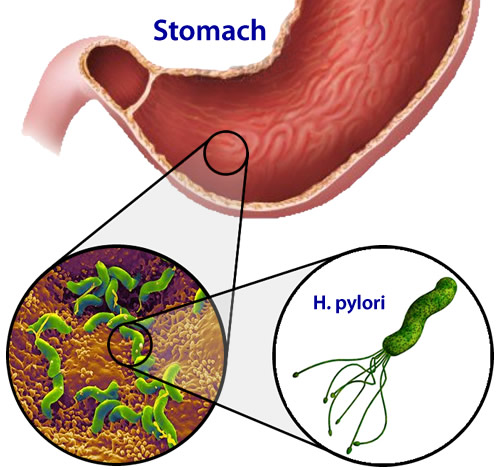
Schwartz's dictum "no acid, no ulcer" still holds true, and gastric acid is necessary for the occurrence of peptic ulcer. Ulcer are extremely rare in the the presence of achlorhydria (absence of acid in stomach), and reduction of acidity accelerate ulcer healing. However since many duodenal ulcer and most gastric ulcer patients secrete normal or subnormal amounts of gastric acid, the role of acid in ulcer pathogenesis is now thought to be contributory rather than causal in most cases. The current understanding is that Helicobacter pylori (H pylori ) is responsible for 95% of duodenal ulcers and 60-80% of gastric ulcers. The strongest evidence for the pathogenic role of H pylori in peptic ulcer disease is the marked decrease in the recurrence rate of ulcers following the eradication of infection. The second most important cause of peptic ulcer is NSAIDs (pain killers). Rare causes of peptic ulcers include pathological hypersecretory conditions such as gastrinoma ( Zollinger-Ellison disease) and duodenal Crohn's disease.
The patient with uncomplicated peptic ulcer usually present with abdominal pain or discomfort. Vomiting, weight changes, and symptoms of anaemia are less common. It is not possible to differentiate between gastric and duodenal ulcers from history alone.

Pain
The pain of peptic ulcer is typically situated in the epigastrium, but may occur in the lower chest or right or left hypochondrium. It is said that ulcer pains can often be localised to a very small area (pointing sign). The pain tends to occur when the patient is hungry, 1 to 3 hours after meals, to wake up patient up at night, to be relieved by food, antacids and vomiting, and also to be characterised by remissions and exacerbations. Some patients may describe their pain as a burning sensation, a discomfort or indigestion. Pain may radiate to the back.
The diagnosis of peptic ulcer cannot be established or excluded on the history alone. Typical ulcer-like pains may occur in a patient without ulcer ( non-ulcer dyspepsia) and conversely, ulcer patients may reports pains which are unrelated to food. Ulcer may be present without causing pain or symptoms. Asymptomatic ulcers are more common in patient taking pain killers and in elderly patients. These patients may present only when complications like bleeding or perforation have occurred.
Vomiting
Vomiting is infrequent in ulcer disease but occur due to oedema and spasm around a pyloric canal ulcer causing gastric outlet obstruction. Chronic prepyloric gastric ulcers and duodenal ulcers sometimes lead to gastric outlet obstruction through fibrosis.
Weight loss
Most ulcer patient do not report any weight change. Occasionally, duodenal ulcer subjects gain weight because eating relieves their pain. Conversely, gastric ulcer patients sometimes lose weight because eating worse their pain.
@myintthein
Great content, thanks for sharing!
Welcome