DRUGS AND PREGNANCY
Hi Steemians!
We are sure you know that certain drugs, even some common medicines like co-trimoxazole (Septrin) and aspirin could pose serious risk to the unborn child if taken during certain stages of pregnancy. The question is how much of such drugs do you know?
Years back, a research showed that nearly 70% of pregnant women are taking a medication in their first trimester (first 3 months of pregnancy) in which the organs of the unborn is developing. If these drugs interfere with pregnancy, there will be an increased risk of abortion, birth deformities and still birth.
SOURCE
Surprisingly, some Vaccines too are contraindicated in pregnancy. Measles, live poliomyelitis and yellow fever vaccines should be avoided during first trimester. For Rubella and MMR vaccines, pregnancy should be avoided for 1 month after immunization while for Varicella vaccine, pregnancy should be avoided for 3 months after immunization.
“How dangerous could the effect of a teratogen ( an agent that causes malformation of an embryo) be?” you may ask.
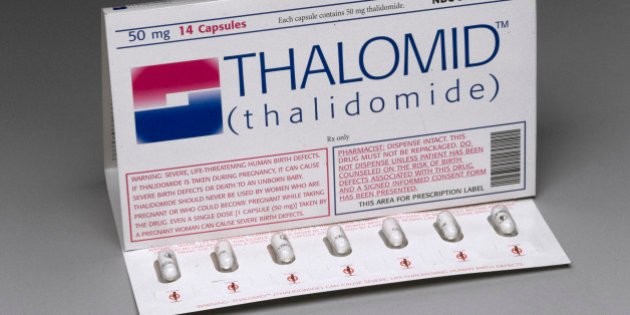
A throwback to the 1960 Thalidomide disaster will answer that.
Thalidomide was first marketed in Germany in 1957 as an over-the-counter drug indicated initially as a treatment for seizures, and later as an anti-nauseant and sedative. Since the manufacturers could not find adverse effects at high doses, they claimed it was completely safe for everyone, including mother and child. According to the Thalidomide Trust, In April, 1958 Thalidomide was licensed for distribution in the UK under the brand name Distaval.
The sedative was promoted as a ‘wonder drug’ to treat a range of conditions including headaches, insomnia and morning sickness in pregnant women – adverts emphasised the drug’s safety using phrases such as ‘non-toxic’ and ‘no known toxicity’. During this period, the use of medications during pregnancy was not strictly controlled, and drugs were not thoroughly tested for potential harm to the fetus.
Thousands of pregnant women took the drug to relieve their symptoms. At the time of the drug's development, scientists did not believe any drug taken by a pregnant woman could pass across the placental barrier and harm the developing fetus, even though the effect of alcohol on foetal development had been documented by case studies on alcoholic mothers since at least 1957.
Within a few years of its use, babies started being born with characteristic limb and organ deformities. In 1961, two independent researchers identified thalidomide as the likely causal agent.source
Many children in the 1960's, like the kindergartner pictured above, were born with phocomelia as a side effect of the drug thalidomide, resulting in the shortening or absence of limbs. (Photo by Leonard McCombe//Time Life Pictures/Getty Images;
SOURCE
What other common drugs should be avoided in pregnancy?
The effects of drugs in pregnancy vary with the trimester. Some are safe in the first trimester only, others are safe in the second and third trimesters only, while others are dangerous only in the third trimester.
Below are examples of common drugs that should be avoided in pregnancy:
- Social drugs and drugs of abuse: Alcohol (regular drinking in the first trimester is teratogenic; causes growth retardation and dependence in fetus), morphine, codeine (suppresses respiration; there are withdrawal symptoms)
- Antihypertensives: ACEIs e.g. Lisinopril and ARBs e.g. Losartan (causes foetal and neonatal kidney dysfunction)
- Anthelmintics: Albendazole, mebendazole (avoid in 3rd trimester)
- Antibiotics: Apart from the penicillins (e.g. ampicillin, amoxicillin), the cephalosporins (e.g. cefixime, cefuroxime, ceftazidime), erythromycin and clindamycin, other antibiotics should be used only when benefit outweighs risk. Ciprofloxacin, ofloxacin (avoid in all trimesters, causes arthropathy), trimethoprim, sulphamethoxazole (folate antagonist, causes neonatal haemolysis), doxycycline, tetracycline (affects skeletal development, causes teeth discolouration),metronidazole, tinidazole (avoid high doses)
- Antifungal: fluconazole (associated with significantly increased risk for spontaneous abortion, avoid), griseofulvin (avoid completely)
- Antimalarials: Primaquine (avoid in third trimester, may cause neonatal haemolysis). Sulphadoxine/pyrimethamine (should not be used during first trimester since it is an anti-folate agent. The WHO recommends it for Intermittent preventive treatment of malaria in pregnancy during the second and third trimester), Quinine (high doses are teratogenic in first trimester; but in malaria benefit of treatment outweighs risk)
- Oxytocics: mifepristone, misoprostol (avoid in all trimesters)
- Antineoplastic agents (Drugs used to treat cancer): Methotrexate, Tamoxifen, cyclophosphamide, doxorubicin (teratogenic).
- Antidiabetics: Glibenclamide (reduced blood sugar in neonates, third trimester), Metformin (avoid in all trimester). Use of Insulin is safer, always seek medical advice.
- Warfarin causes fetal intacerebral bleeding.
- Hormonals eg medroxyprogesterone can cause inappropriate virilization or feminization of child.
- Isotretinoin (avoid completely, severe teratogenic effects as serious craniofacial, cardiovascular, thymic and central nervous system malformations.
There are still other medicines which are not safe for use in pregnancy. Infact, medication use during pregnancy is totally discouraged as all drugs are assumed harmful until proven otherwise. This is because experience with many drugs in pregnancy is severely limited due to paucity of and difficulties in research in this area.
From the researches carried out so far, drugs are classified into the following categories based on their risk potential to pregnancy:
Category A: No risk from controlled studies in pregnant women, evidence of harm not found. Medication is safe.
Category B: No risk found in animal studies and no controlled studies in pregnant women; or no studies in animals and pregnant women. Medication may be safe.
Category C: Risk found in animal studies but no controlled studies in pregnant women. Safety is not guaranteed.
Category D: Positive evidence of fetal risk in human studies, but benefits of use in life threatening condition to mother may be accepted despite risk. Avoid except benefit outweighs risk.
Category X: Positive evidence of fetal risk in animals and pregnant women; risk of use clearly outweighs risk. Avoid.
In conclusion, we advice that medications should not be taken carelessly during pregnancy to avoid unforeseen harm to the mother and fetus. All mediactions taken during pregnancy should be prescribed by the Doctor and advice/additional information should be gotten from the Pharmacist when necessary.
ADDITIONAL SOURCES
Ritter, JM. etal (2008), A Textbook of Clinical Pharmacy and Therapeutics, 5th Edition. pg 45-48
Medscape
Emdex
Martindale

Hello @drugcompendium, upv0t3
This is a free service for new steemit users, to support them and motivate them to continue generating valuable content for the community.
<3 This is a heart, or an ice cream, you choose.
:)
R4ND0M:
3376 5504 6411 8846
5828 4819 8723 8817
9896 8402 1592 6272
7330 2450 1939 4680
This is a lovely nice read. Insightful to the fullest. I believe the general public needs to be enlightened on the dangers of some medications during pregnancy and consult their physicians or pharmacists as the case may before drug administration.