Conficker's Journal #1; Peritonsillar Abscess

Hi guys,
It's been awhile since my last article. I have decided to start my own series featuring medical cases which I have encountered throughout my career as a medical doctor. In this first series, we would discuss a case which is related to Peritonsillar Abscess. Throughout the discussion, I would be using a pseudonym in order to protect the identity of my patient. I would try my best to explain any medical-related terms so that every reader would earn something from this article.
Introduction
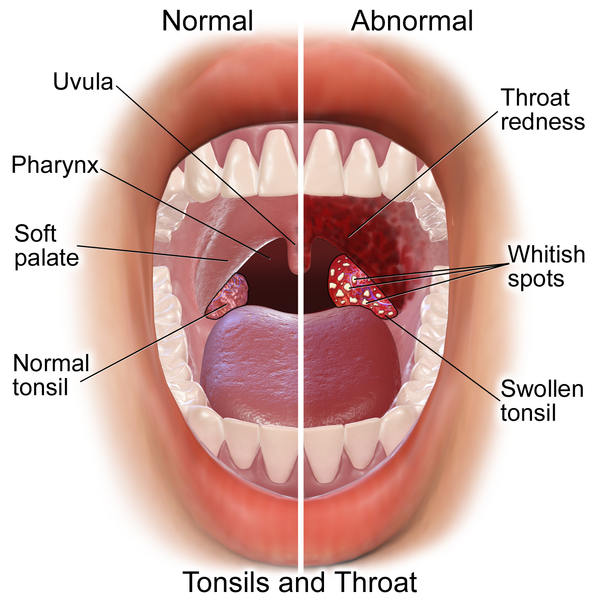
To understand about Peritonsillar Abscess, you need to know what exactly is Peritonsillar. The name of the disease itself is self-explanatory. Peritonsillar concern with the location of the disease and Abscess describe an accumulation of pus within the tissue in the body. So where exactly is Peritonsillar? So peritonsillar area is located in between two structure in the oral cavity. On the medial side is the palatine tonsillar capsule while on the lateral side is the superior pharyngeal constrictor muscle. Basically, Peritonsillar Abscess or PTA is the accumulation of pus in the tissue located in between those two structures which we called the peritonsillar area.
There are two types of Peritonsillar Abscess:
- Unilateral Peritonsillar Abscess
- Bilateral Peritonsillar Abscess
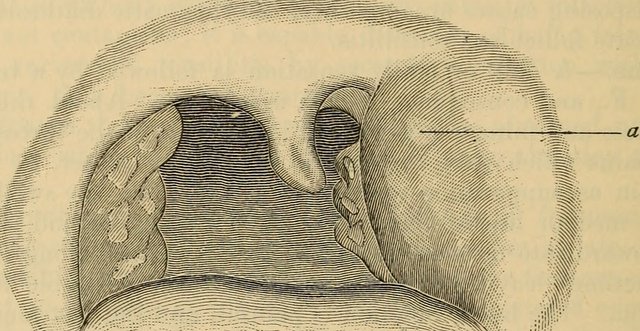
The picture above shows an example of a unilateral Peritonsillar Abscess. The organ located just posterior to the structure labelled "a" is the tonsil. So basically, the affected side would be swollen, filled with pus and tender.
Peritonsillar Abscess is generally common among adolescents and young adults. The incident of Peritonsillar Abscess among infants and young children (below 12 years old) were usually rare but if they presented with the signs and symptoms which could suggest Peritonsillar Abscess, it should not be excluded from the differential diagnosis. Most of the elderly patients who have been diagnosed with this disease have histories of prolonged hospital stay. It's a significant ailment among the elderly as it gives rise a greater percentage of morbidity and mortality rate compared to the pediatric population.
In most cases, Peritonsillar Abscess was formed as a result of monomicrobial insult (caused by a single species of bacteria) but in the past, there are some specimens which yield a polymicrobial pattern of growth suggestive of a combination of bacteria which affect the development of the disease. There are a few theories regarding the pathogenesis of Peritonsillar Abscess but only two were widely accepted:
- Complication of acute bacterial tonsilitis
- Complication of salivary gland infection
There are a few studies that have been conducted in the past which found that Peritonsillar Abscess can be the result of a post-tonsillectomy complication. Tonsillectomy is a surgical procedure to remove the tonsils. Whatever it is, Peritonsillar Abscess seems to affect chronic smokers. This can be due to a few factors such as:
- Gingival mucosa atrophy
- Alteration in the flora of the oral cavity
- Reduced oral immunity
Case Study

Last week, I have the opportunity to interview and examine a patient which has been admitted due to Peritonsillar Abscess. Derek (pseudonym) is a 24 years old male who came to the ENT clinic with a chief complaint of a sore throat and painful swallowing (odynophagia) for 6 days duration. Apparently, both of this symptoms were accompanied by few more which are:
- Low-grade fever
- Limited mouth opening (trismus)
- Muffled voice
- Ear pain (otalgia)
- Reduce oral intake
According to him, everything seems fine until 6 days ago, when a sore throat started along with odynophagia and reduce oral intake. The other symptoms mostly appear 1 day prior to the day he was admitted. He lost a quite significant amount of weight and seems fatigue as he can't eat, drink and sleep well. He shows some symptoms which could indicate mild dehydration but I figured that was fine. Throughout the 6 days, he had to use a Difflam spray before he can eat. Difflam spray is a local analgesic which is usually used in a condition which involves painful mouth or throat as a part of the disease process.
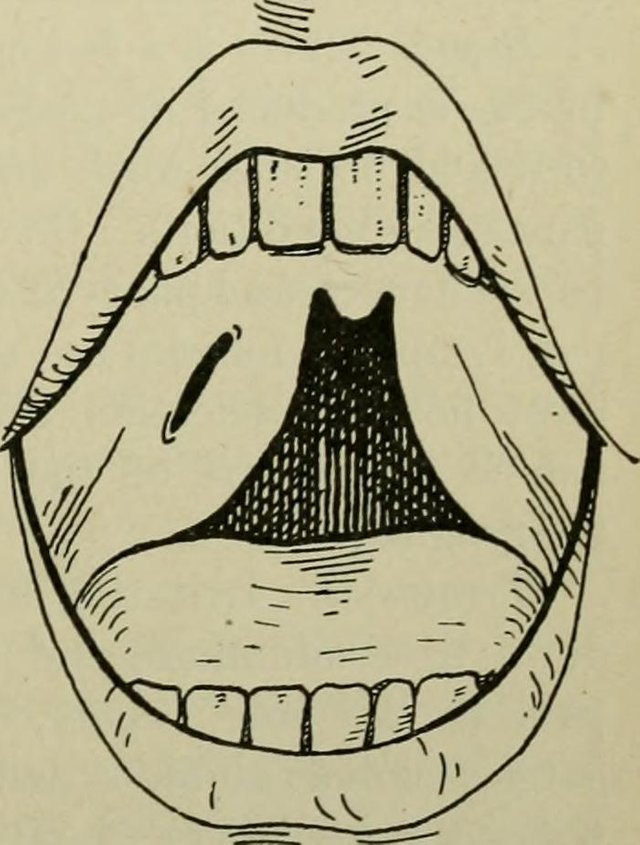
It was difficult. He struggled to communicate with his friends due to the trismus (limited mouth opening) and the muffled voice. While I was clerking him, sometimes, he had to write in a piece of paper to communicate with me. If you are not familiar with the muffled voice, you can refer to the video.
For your information, all of the symptoms experienced by Derek were classical for the diagnosis of Peritonsillar Abscess. However, the history should be reconfirmed with oral examination and some investigations if it was deemed necessary. Oral examination done revealed a left peritonsillar swelling which is erythematous (red) and quite tender. Immediately after the findings, Derek was asked to go to a treatment for a procedure called Incision and Drainage(I&D). For a Peritonsillar Abscess, it was important to drain the pus as soon as they were discovered to ensure a quicker recovery.
The first attempt of I&D doesn't yield any pus which makes us suspicious whether or not this is a Peritonsillar Abscess. As there were no evidence it was an abscess, the diagnosis was changed to Peritonsillitis; inflammation of the peritonsillar area which is commonly caused by an acute tonsilitis. However, after he was admitted for two days, pus was liberated while I&D was performed which confirmed the initial diagnosis of Peritonsillar Abscess.
Discussion and Treatment

Derek was diagnosed with a unilateral Peritonsillar Abscess which has been completely evacuated after 3 sessions of I&D. Mind you, this kind of procedure is quite painful even with the local analgesic. Initially, Derek requested for the I&D to be performed under General Anaesthesia but as it turns out, it was irrelevant due to a few reasons:
- He had trismus so it would be difficult to intubate him
- General anaesthesia poses a much more side effect compared to the local anaesthesia for this procedure.
Recognising Peritonsillar Abscess is quite important as it can lead to various complications if they were missed. In a study conducted by Chung et al in 2014 has revealed that without proper intervention, the infection could spread out to a few structures such as epiglottis and larynx, the base of the skull and the retropharyngeal space before it will be aspirated and cause airway obstruction hence sleep apnea. The recurrence rate of tonsilitis would also be determined by the extent of spread from the focus of infection (peritonsillar area). It is worth noting that, if the extent of spread is significant, the rate of recurrence can be up to 22.7%.
There are a lot of treatment modalities that can be chosen in order to treat Peritonsillar Abscess. According to Tachibana, the rate of recovery will depend on three important factors which are:
- Age (Older age is associated with a longer period of recovery)
- The level of C-reactive protein
- Delayed drainage procedure
The third factor implies the importance of an early drainage to achieve a better disease outcome in a shorter period of time. Some patients can be treated conservatively with a 7 days course of antibiotic, while the others, have to be treated with either:
- Needle aspiration
- Incision and drainage
- Quinsy tonsillectomy
There is no general consensus or even a guideline which could tell a clinician regarding the priority of treatment among patients with Peritonsillar Abscess; it would depend on the clinician's judgement and skill. However, if a patient was treated conservatively with antibiotics, they need to be reminded to inform if the symptoms are not resolved within 3 days; at that point, surgical intervention was necessary.
Treatment actually is the easiest part. Recognising Peritonsillar Abscess can sometimes be tricky especially when it is a bilateral Peritonsillar Abscess. It can be considered as an emergency case as, without a proper intervention, the patient won't be able to breathe due to obstruction of the respiratory tract. There are a few key signs which you would not find in a bilateral Peritonsillar Abscess such as:
- Uvula deviation (as both peritonsillar areas are swollen)
- Unilateral referred ear pain
- Asymmetrical tonsils/palate size
All three of the signs mentioned above can give important clues whether the patient is having a Peritonsillar Abscess or not and without it, clinicians often misdiagnosed.
Derek was discharged 5 days after admission with a few antibiotics. to be completed by him in 7 days. The case might seem simple but it is important, as, without treatment, it can lead to a few complications which might be life-threatening for Derek.
Sources
- Prognostic factors and effects of early surgical drainage in patients with peritonsillar abscess.
- Peritonsillar infections: local experience.
- Epidemiology, clinical history and microbiology of peritonsillar abscess.
- Risk factors for recurrence of peritonsillar abscess.
- Bilateral Peritonsillar Abscesses: A Case Presentation and Review of the Current Literature with regard to the Controversies in Diagnosis and Treatment.
- Bilateral peritonsillar abscess: A case report and pertinent literature review


SteemSTEM is a community project with the goal to promote and support Science, Technology, Engineering and Mathematics on the Steem blockchain. If you wish to support the steemSTEM project you can:
Contribute STEM content using the #steemstem tag | Support steemstem authors | Join our curation trail | Visit our Discord community | Delegate SP to steemstem
Very interesting and I’m really hoping I never get a peritonsillar abscess - sounds painful!
I was interested in the statement about rate of recovery being dependent on C-Reactive protein (CRP) status. I’m assuming you mean if CRP is high then recovery will be slowed and if it’s low recovery will be hastened.
I’m guessing that is because CRP is an indicator of inflammation in the body - so if it’s fighting inflammation elsewhere or systemically the immune system just doesn’t have the resources to fight it all. Am I on the right track?
And would the abscess itself (or alone) cause an increase in CRP?
It’s a blood marker I find very interesting. Especially since In certain people (like obese people) where I would expect it to be high because of the inflammation inherent in being overweight - it sometimes comes back low.
Is there a genetic component to the marker? Inquiring minds and all that.
Looking forward to following!
Well from what I understand about CRP is they are the marker of inflammation which is produced by the liver. It doesn't fight inflammation, it just indicates there is a high level of inflammation in the body which can be due to infection and other inflammatory processes.
Abscesses were caused by infections, so yeah, CRP does increase when there is an abscess. In fact, there are some journals published which described the importance of CRP in differentiating between the diagnosis of brain abscess and brain tumour. However, CRP is a non-specific marker which kinda unreliable.
I'm not sure whether the rate of production of CRP will be genetically affected or not. Any processes which caused an elevated CRP level were usually associated with a poor healing process.
This is one of those articles with a high rate of "ewwiness". But you are most probably rugged in that and it's only business for you. My mother is a MD. I don't know much about it but reading your article made my tonsils hurt. My better half has had her tonsils removed and she is very prone to throat infections and irritations even after eating an ice-cream or drinking cold juice on a summer day.
The conclusion is nobody wants infections in their body and the timely detection and treatment is obviously how anyone should proceed, instead of self medicating.
In Europe we do have a problem with self medication. The consumption of antibiotics has reached an all time high. You can generally get any antibiotic, including the reserve antibiotics without prescription if you try to haggle with the pharmacists a little.
The articles is written in a professional way, clearly even better than the one before, and the content is structured and personal, since you have used Derek. I hope he is OK now. You just need to link it in the community by tagging other medical personnel who might have something to add or to talk about their personal experiences and you are set.
Cheers!
Thanks, @alexdory for the feedback. :)
@bbkivines is a resteem bot follow and send 0.50 SBD and get daily votes and resteems
It is nice to see another science educator here. I'm just beginning, but hope to build collection of technical leaning materials physics posts here.
Hi @spbeckman. Good luck and I pray you will succeed in promoting physics-related content here, on Steemit.