Awareness about an Eyes Disease ''Keratoconus''
MY PERSONAL EXPERIENCE
Today I am going to tell you my story something like personal experience I just finished my engineering when I was in 5th semester I continuously feeling headache in my head first I just ignore it thinking that it is maybe the reason not sleeping very well or something like that but I notice it for about two months then I share this problem with my friend he thinks it maybe cause of your eyesight he took appointment from a doctor which was an eyes specialist when the doctor examined my eyes I just shocked OMG what is this my right side eye, its 80 percent not working I didn't see anything on it everything was completely blurred to me then the doctor suggest me to use glasses so from that time I starts wearing glasses regularly I was thinking that like all other people who uses glasses I will be just like them nothing more but with the glasses my headache is disappeared more than enough but after a month I realized that my headache is not like before but I cant see clearly on my right side eye still with the glasses also so I start going to doctors again every doctor suggests me a different number of glasses... I just sick of this problem then recently I got an appointment from another doctor he examined me very well and finally diagnose the disease of mine and that disease is called Keratoconus.
NOTE:
Firstly my advice is to all yo have to go to the doctor which have a complete experience..otherwise you will be going worse day by day and no doctor will diagnose what problem you are having.
so have to find a good doctor first!
Now I am going to tell you about
'' WHAT IS KERATOCONUS? ''
Keratoconus Symptoms:
The KC cornea shape is very much different than that of the normal one.
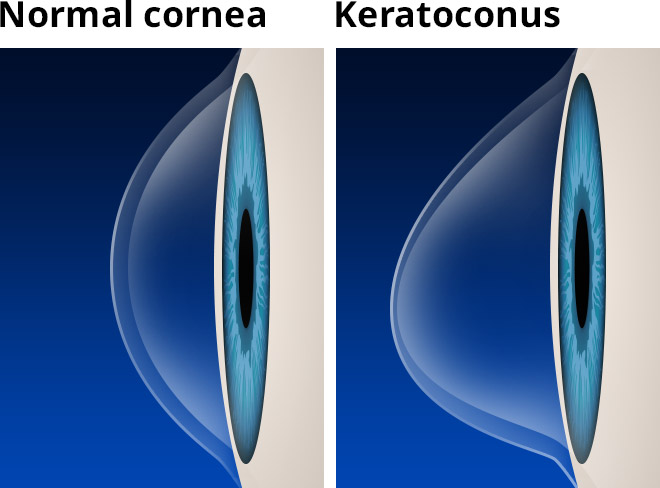
The earliest signs of keratoconus are usually blurred vision and frequent changes in eye glass prescription, or vision that cannot be corrected with glasses. Symptoms of keratoconus generally begin in late teenage years or early twenties, but can start at any time.

 ,
, 

Keratoconus can cause these kinds of visual distortions. Common symptoms like those pictured are: ghosting, multiple images, glare, halos, starbursts around lights and blurred vision.
Other symptoms include:
Increased light sensitivity
Difficultly driving at night
A halo around lights and ghosting (especially at night)
Eye strain
Headaches and general eye pain
Eye irritation, excessive eye rubbing.

Images courtesy of Ian McCain and
Elio Spinello, kcvision.org
Keratoconus, especially in the early stages can be difficult to diagnose and all of the above symptoms could be associated with other eye problems. Simply recognizing symptoms does not by itself diagnose keratoconus.
Keratoconus requires a diagnosis from a competent eye doctor trained not only in recognizing the symptoms but also observing signs of keratoconus through direct measurement as well as inspection of the cornea at a microscopic level using a slit lamp.
Always consult your doctor to confirm a diagnosis of Keratoconus.
Keratoconus Diagnosis & Treatment
Keratoconus can usually be diagnosed with a slit-lamp examination. The classic signs of keratoconus that the doctor will see when examining your eyes include:
Corneal thinning
Fleischer’s ring (an iron colored ring surrounding the cone)
Vogt’s striae (stress lines caused by corneal thinning)
Apical scarring (scarring at the apex of the cone)
The doctor will also measure the curvature of the cornea this is done by:
Keratometry: An instrument that shines a pattern of light onto the cornea. The shape of the reflection of the pattern tells the doctor how the eye is curved.
Corneal topography: a computerized instrument that make three-dimensional “maps” of the cornea.
A typical corneal topography map looks like this:

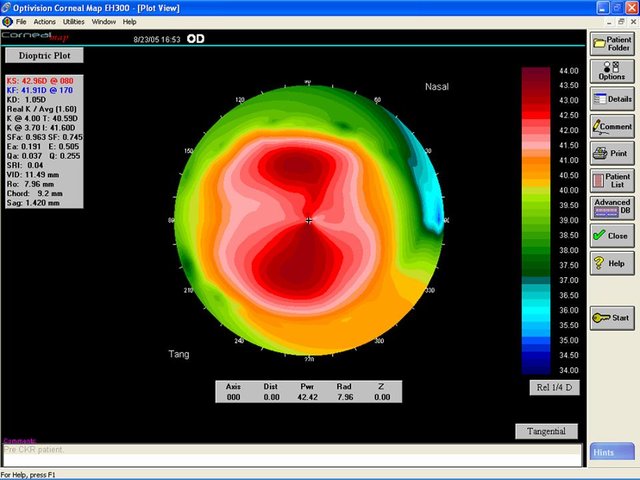
Corneal topography has facilitated the diagnosis of keratoconus, helping establish the diagnosis earlier, follow progression more accurately and differentiate keratoconus from other conditions.
Treatments
Contact Lenses for KC
There is no one design that is best for every type or stage of keratoconus. The “best lens” is the one that fits your eye, corrects your visionand is comfortable to wear. Rely on an experienced KC lens fitter to select the best lens for your eye.The needs of each individual is carefully weighed to find the lens that offers the best combination of visual acuity, comfort and corneal health Contact lens fitting for keratoconus is part science and part art. A great deal of patience is required both on the part of the fitter and the patient.
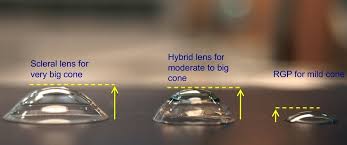
Here is a brief outline of the types of lenses available for keratoconus:
Soft Lenses
The role of soft lenses for Keratoconus vision correction has changed dramatically in the past year. The new soft lens designs combine the latest technologies in silicone hydrogel materials and complex mathematics to offer comfortable wear and excellent vision.

Older soft lenses draped over the irregular Keratoconus cornea assuming the same irregular surface as the KC cornea without correcting the visual distortion caused by the irregularly shaped KC cornea.

RGP Contact Lenses
Rigid Gas Permeable (RGP or GP) contact lenses are primary option for correcting KC vision. The rigid lens masks the underlying irregular cornea and functions as the new refractive surface of the eye, with the tear film filling in the space between the back of the contact lens andthe front of the eye. “Rigid” defines the type of lens. “Gas Permeable” describes the lens material. There are many different RGP lens designs.
Piggy-backs
This is a two lens system; an RGP lens worn on top of a soft lens. The RGP lens provides crisp vision and the soft lens acts as a cushion providing comfort.

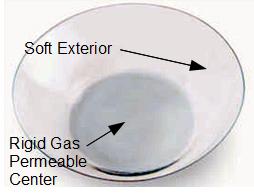
Hybrid lenses
Hybrid-contacts this is a lens design combination that has an RGP center surrounded by a soft peripheral “skirt”. Hybrid contact can provide the crisp optics of a GP lens and wearing comfort of soft contact lenses. They are available in a wide variety of parameters to provide a fit that conforms well to the irregular shape of a keratoconic eye.
Scleral lenses
These are large diameter lenses that rest on the white part of the eye, called the sclera, and vaults over the cornea. The size can be an alarming prospect for some, but scleral lenses have many advantages. Because of their size, they do not fall out and dust or dirt particles cannot get under them during wear. They are surprisingly comfortable to wear because the edges of the lens rests above and below the eye lid margins so there is no lens awareness. The introduction of rigid gas permeable (RGP) materials has made this design more readily available.
 ,
, 
Intacs Surgery for Keratoconus
Intacs is the trademark name for micro-thin prescription inserts which were previously used as a form of refractive surgery in the treatment of low levels of myopia or nearsightedness, but has recently received FDA approval for keratoconus. Intacs are thin plastic, semi-circular rings inserted into the mid layer of the cornea. When inserted in the keratoconus cornea they flatten the cornea, changing the shape and location of the cone.
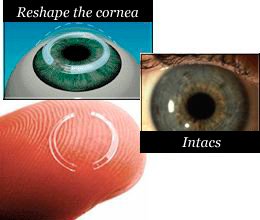 ,
,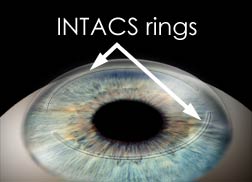 The placement of Intacs remodels and reinforces the cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide improved vision. This can improve uncorrected vision, however, depending on the severity of the KC, glasses or contact lenses may still be needed for functional vision.
The placement of Intacs remodels and reinforces the cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide improved vision. This can improve uncorrected vision, however, depending on the severity of the KC, glasses or contact lenses may still be needed for functional vision.
FDA Approval Intacs were approved under a Humanitarian Device Exemption (HDE) by the FDA in July 2004, allowing Intacs to be used for treating keratoconus. As part of the HDE approval, Addition Technology, the manufacturer of Intacs, has implemented an extensive training program in which each surgeon will be required to participate. What is a Humanitarian Device Exemption (HDE)? The humanitarian device regulations were first established in October 1994. Humanitarian Use Devices (HUDs) are medical devices specially designated by the FDA for use in the treatment of fewer than 4000 patients per year with rare medical conditions. CPT Code is: Category III CPT code 0099T Intacs received a Category III CPT code 0099T from the American Medical Association. Category III CPT codes are codes to designate emerging technologies and are not assigned a value. It is up to the insurance company to determine the amount to be paid.
Intacs | Corneal Implants
This procedure involves placing the plastic inserts just beneath the surface of the eye in the periphery of the cornea. The procedure itself takes approximately 15 to 20 minutes usually in the doctor’s office. Topical anesthetic drops are used to numb the eye, and a clamp is used to hold the eye open throughout the procedure to prevent blinking. There are 3 basic steps to the procedure: Step 1: A single, small incision is made in the surface of the cornea. Instead of using mechanical cutting, some surgeons may use a laser to make the incision. Step 2: A centering guide is placed on the surface of the eye for several minutes to help stabilize the eye and ensure proper alignment of the Intacs insert. During this time, the corneal layers are gently separated in a narrow circular band on the outer edge where the Intacs will be placed. Step 3: The Intacs inserts are placed. Once this insertion is completed, the small opening in the cornea is closed with a suture. Follow-up visits will be required to monitor the healing process and to evaluate the visual benefits of the procedure. Even after a successful procedure, glasses or contacts may be required. As with any surgical procedure, there are some risks, including infection. Some patients experience visual symptoms including difficulty with night vision, glare, halos, blurry and fluctuating vision. For more information go to: www.intacsforkeratoconus.com
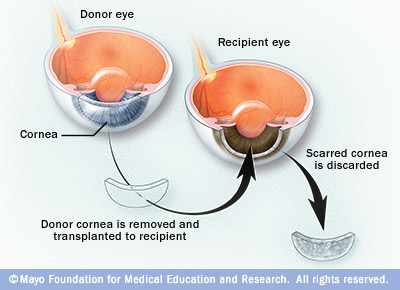
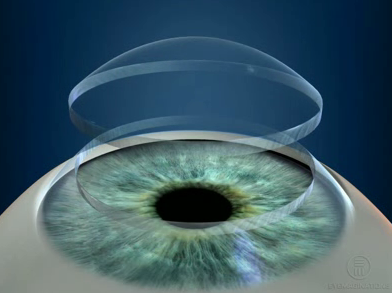
Corneal Transplants
Although only 15-20% of those with keratoconus ultimately require corneal transplant surgery, for those who do, it is a crucial and sometimes frightening decision. However, those who know what to expect before, during and after surgery are better prepared and feel more in control of their health care.corneal transplant surgery In keratoconus, a corneal transplant is warranted when the cornea becomes dangerously thin or when sufficient visual acuity to meet the individual’s needs can no longer be achieved by contact lenses due to steepening of the cornea, scaring or lens intolerance. Lens intolerance occurs when the steepened, irregular cornea can no longer be fitted with a contact lens, or the patient cannot tolerate the lens.To receive our Corneal Transplant Booklet, please fill out our form here.''
 ,
,