Klasifikasi
Hypoxic Hypoxia
Where PO2 artery blood is reduced. Hypoxic hypoxia is a hypoxic state caused by lack of oxygen entering the lungs so that oxygen can not reach the blood and fail to enter the blood circulation. This failure can be caused by obstruction or obstruction in the respiratory tract, either by natural causes (eg disease accompanied by respiratory blockage such as diphtheria laryngitis, asthmatic status, carcinoma and so on) or by mechanical trauma or violence, such as airway obstruction, choking, hanging, drowning and so on.
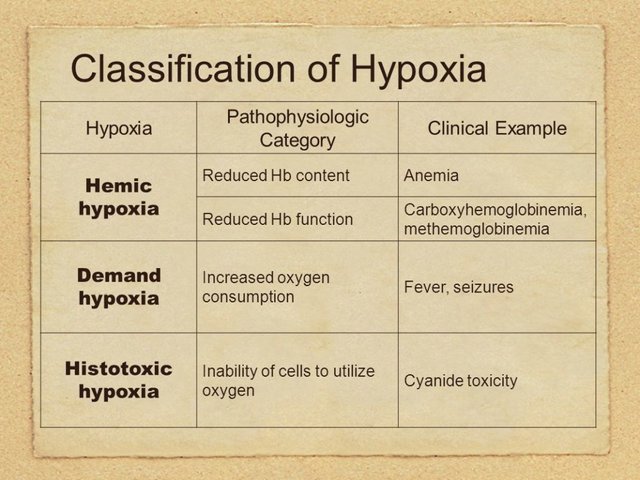
Anemic Hypoxia
Where arterial blood PO2 is normal but the amount of hemoglobin available to transport oxygen is reduced, as in carbon monoxide poisoning because the CO affinity for hemoglobin is much higher than that of oxygen affinity with hemoglobin.
Stagnant Hypoxia
Hypoxia stagnant is a hypoxic state caused by blood (hemoglobin) is unable to carry oxygen to the tissues due to circulatory failure such as heart failure or embolism, both venous air embolism and fat embolism even though PO2 is a normal hemoglobin concentration.
Hypothoxic Hypoxia
Where the amount of oxygen delivered to a tissue is adequate but due to the action of substances toxic tissue cells can not use the oxygen provided, for example in cyanide poisoning. Cyanide in the body will activate some radical tissue oxidative enzymes radically especially cytochrome oxidase by binding to the ferricheme group part of the blood-borne oxygen. Thus, the oxidation-reduction process in the cell can not take place and oxyhemoglobin can not dissociate release of oxygen to tissue cells resulting in tissue hypoxia. This is a paradoxical condition, because the victim dies cyanide poisoning hypoxia though in his blood rich in oxygen.
Pathophysiology
In a state of consciousness such as anesthesia, head trauma / illness, relaxation of the muscles, including the tongue muscle as a result when the patient's position is supine, the base of the tongue will fall posteriorly to the oropharynx, causing airway obstruction. Sphincter cardia is relaxed, causing the contents of the stomach to flow back into the oropharynx (regurgitation). This is a threat of airway obstruction by dense aspirate and aspiration of pneumonia by aspiration of liquid, because in this condition generally reflex cough has decreased or disappeared.
Respiratory failure includes oxygenation failure and ventilation failure. Oxygenation failure may be caused by:
imbalance between ventilation and perfusion.
a right-left intrapulmonary blood short-circuit.
low pulmonary venous oxygen tension due to inadequate inspiration, or due to mixed oxygen-containing blood.
diffusion disorder of the alveolar capillary membrane.
hypoventilation of the alveoler.
Ventilatory failure may occur when PaCO2 rises and pH is less than 7.35. Ventilation failure occurs when minute ventilation is reduced unreasonably or if it can not increase in an effort to compensate for increased CO2 production or cavity formation in the event of a dead space. Fatigue of the respiratory muscles / weakness of the respiratory muscles arises when the inspiratory muscles, especially the diaphragm, are unable to generate the pressure required to maintain adequate ventilation. Early signs of exhaustion of the inspiratory muscles often precede a significant decrease in alveolar ventilation resulting in a rise in PaCO2. Initial stages of shallow and rapid respiration followed by uncoordinated inspired muscle activity of respiratory alteration (chest and abdominal respiratory turns), and paradoxal abdominal movement (inward motion of the abdominal wall during inspiration) may indicate moderate respiratory acidosis threatening and stopping breathing.