Wakayama symposium: interface between innate and adaptive immunity in dry eye disease
Full reseach paper Download now from google drive
Kyung-Sun Na1 , Kyu-Yeon Hwang2 , Hyun-Soo Lee3 , So-Hyang Chung3 , Jee Won Mok4 and Choun-Ki Joo3,4*
Abstract
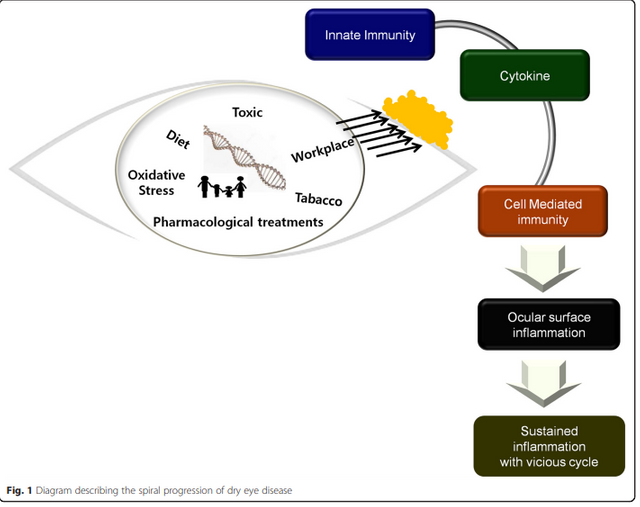
Although the mechanism of dry eye disease is not clearly understood, it is certain that inflammation and the immune response play a major role in determining the health of the ocular surface in dry eye patients. Accurate ocular surface characterization during the early stages of dry eye disease is critical for successful treatment, because there exists no single standard, objective test to diagnose the early phase of dry eye disease. The treatment target should be direct to prevent the perpetuation of chronic inflammation and immune responses. Numerous studies have categorized dry eye disease as an autoimmune-related inflammatory disease. However, relatively little is known about how innate immune mechanisms act following a local insult, why some patients are particularly vulnerable, and why local inflammation fails to resolve in these patients. Within this review, particular attention will be given to the very early events and corresponding defense mechanism in dry eye disease. The transition from innate to adaptive immunity will also be discussed
Background
The tear film, lacrimal glands, corneal and conjunctival epithelia, and meibomian glands constitute a lacrimal function unit (LFU) that serves to preserve the health of the ocular surface. The components of the LFU work together to maintain homeostasis despite internal and external insults [1, 2]. Dry eye disease (DED) is a highly prevalent inflammatory disease of the LFU that is multifactorial in nature. The definition of DED has evolved from mere tear deficiency to chronic inflammation and the resultant immunologic responses [3, 4]. Whether the inflammation is a cause or result of DED remains to be elucidated. The mechanisms explaining how and when homeostasis is disrupted following local insult or inflammation of the ocular surface are unclear. The immune reaction comprises innate and adapted immunity, which differ vastly in terms of methodology as well as objective. Recent research has examined how the innate immune system influences adaptive immune
responses [5]. Understanding the interface between innate and adaptive immunity would help to define the factors that trigger the adaptive immune response and allow for analysis of autoimmune and allergic diseases from a new perspective. Although the immunopathologic events that sustain the systemic adaptive immune response in DED have been characterized, the stressor that triggers the innate immune response and the interface between innate and adaptive immune mechanisms are not well defined. If the complicated crosstalk between innate sensory function and the adaptive response at the ocular surface could be understood, the pathogenesis of DED would be clearer. We aimed to briefly review the clues of innate immunity and the interface between innate and adaptive immunity in DED.
Full reseach paper Download now from google drive
This article is distributed under the terms of the Creative Commons Attribution 4.0
Creative common public domain dedication