Everything you need to know about Depression (Major Depressive Disorder)
What is Depression?
As a widespread and significant medical ailment, depression (a major mental condition) impacts one's mood, thinking patterns, and behavior. Because illness is curable, it is a blessing. It is characterized by persistent grief or a diminished interest in once-enjoyable pursuits. Several mental and physical health issues might result, making it difficult to carry out daily tasks at work or home.
Conditions/Diseases that can get worse if you have depression:
- Diabetes
- Arthritis
- Cancer
- Asthma
- COPD ( Emphysema & Chronic Bronchitis)
- Obesity
- Cardiovascular Disease
- Irregular Menstrual Cycle
- PCOS
- Bipolar Disorder
Top 10 Symptoms of Depression
Depression symptoms can vary from mild to severe and can include:
- Sad feelings, depressed mood, tearfulness, emptiness, or hopelessness
- Anger outbursts, irritability or frustration, even over small matters
- Having a sense of shame or guilt
- Loss of interest in previously enjoyed activities, we might lose interest in things we used to enjoy like sex, hobbies, and *sports.
- Feeling worthlessness, Increased tiredness, or exhaustion.
- Unrelated weight loss or gain due to changes in appetite
- Not being able to sleep well, insomnia, or sleeping excessively.
- The capacity to sit still, pacing, hand-wringing, or otherwise slowing one's motions or voice may indicate an increase in pointless physical activity (these actions must be severe enough to be observable by others)
- Having trouble focusing, thinking clearly, or making judgments
- thoughts of harming yourself like suicidal thoughts
For a diagnosis, symptoms must endure for at least two weeks and show a change in your previous level of functioning.
Also, medical conditions (e.g., thyroid issues, a brain tumor, or vitamin deficiency) can resemble depression symptoms; therefore, it is critical to rule out general medical conditions.
Depression affects an estimated one in fifteen people (6.7%) annually. In addition, one in six individuals (16.6%) will experience depression at some point in their lives. It can occur at any age but typically manifests between the late teens and early twenties. It is more prevalent in women than in men. According to some research, one-third of women experience a major depressive episode over their lifetime. When first-degree relatives (parents/children/siblings) develop depression, the heritability is significant (about 40%).
Symptoms of depression are different among males, females, children, and teens.
Symptoms of Depression in Males
Males may experience symptoms related to their
- Moods include anger, aggression, irritability, anxiety, or restlessness.
- Emotional well-being, such as feeling empty, sad, or hopeless.
- Behavior includes loss of interest, no longer finding pleasure in favorite activities, feeling tired quickly, thoughts of suicide, drinking too much, using drugs, or doing high-risk activities.
- Sexual interest, such as decreased sexual desire or poor sexual performance. Cognitive abilities, such as being unable to concentrate.
- Sleep patterns include insomnia, restless sleep, oversleeping, or not sleeping through the night.
- Physical health, such as fatigue, pains, headaches, or digestive problems; and mental health, such as depression, anxiety, or irritability.
Symptoms of Depression in Females
Females may experience symptoms related to their
- mood, such as a bad temper
- Emotional health, like feeling sad or empty, worried, or without hope.
- Behavior, like losing interest in things, pulling away from people, or having suicidal thoughts.
- cognitive skills, like being able to think or speak more slowly
- Sleep patterns, like not being able to sleep all night, waking up early, or sleeping too much.
- Physical health, like less energy, more fatigue, changes in appetite, changes in weight, aches, pain, headaches, or more cramps.
Symptoms of Depression in Children
Children may experience symptoms related to their
- Mood, like irritation, anger, mood swings, or crying.
- Behavior, like getting in trouble at school or refusing to go, avoiding friends or siblings, having thoughts of death or suicide, or hurting oneself.
- Cognitive abilities, like having trouble focusing, doing worse in school, or changing grades.
- patterns of sleep, like not being able to sleep or sleeping too much
- Physical health, like lack of energy, stomach problems, changes in appetite, or loss or gain of weight.
Major Causes of Depression
Causes may vary from person to person, but here is an overview of all causes.
- Personality: People who are easily overwhelmed or who struggle to cope may be inclined to depression.
- Age: Senior citizens are more likely to suffer from depression. Other factors, such as living alone and lacking social support, can worsen this.
Women are nearly twice as likely as men to develop depression. Nobody knows why. The hormonal changes that women experience at various stages of their lives may be a factor. - Medication: Depression is a side effect of some medications. Recreational drugs and alcohol can also cause or worsen depression.
- Brain Chemistry: Changes in brain chemical levels can cause depression.
- Genetics: If you have a depressed relative, you are more likely to develop depression.
Chronic physical pain and illnesses can contribute to it. People with a depressive disorder are more likely to have diabetes, cancer, or Parkinson's disease. - Stress: the death of a loved one, upsetting events (trauma), isolation, and a lack of support can all contribute to depressive disorder.
Treatment of Depression
You may successfully mimic the symptoms of depression with a single treatment or require a combination of treatments. A psychiatrist may prescribe medication for depression treatment or give you advice for treatment.
Medication
Your doctor may prescribe medication for depression treatment , including
Selective Serotonin Reuptake Inhibitors (SSRIs)
Selective serotonin reuptake inhibitors (SSRIs) are widely prescribed medication therapies for the treatment and eradication of the symptoms of depression. These medications have fewer side effects than other types of medication therapy.
SSRIs are not compatible if given with other drugs such as monoamine oxidase inhibitors (MAOIs), norepinephrine reuptake inhibitors (SNRIs), theophylline ( an asthmatic medication), and some NSAIDs ( Ibuprofen, diclofenac, and naproxen).
SSRI for depression treatment
Some common examples of SSRIs are paroxetine (Paxil), fluoxetine (Prozac), citalopram (Celexa), escitalopram (Lexapro), and sertraline (Zoloft).
Serotonin and norepinephrine reuptake inhibitors (SNRIs)
SNRIs cure depression by boosting the neurotransmitters serotonin and norepinephrine in the brain. They're also used to treat anxiety, obsessive-compulsive disorder (OCD), attention deficit hyperactivity disorder (ADHD), fibromyalgia, nerve pain, and other pain disorders, among other things.
When taking MAOIs and SNRIs together, you should use caution if you have liver or renal problems or narrow-angle glaucoma.
SNRI for depression treatment
Desvenlafaxine (Pristiq, Khedezla), duloxetine (Cymbalta, Irenka), levomilnacipran (Fetzima), milnacipran (Savella), and venlafaxine are examples of SNRIs (Effexor XR).
Tricyclic and tetracyclic antidepressants (TCAs and TeCAs)
Tricyclic and tetracyclic antidepressants (TCAs and TECAs) cure depression by boosting the levels of the neurotransmitters serotonin and norepinephrine in the brain. These might be good options for you.
TCAs have a higher risk of side effects than SSRIs or SNRIs. TCAs and TECAs should not be used with MAOIs. If you have narrow-angle glaucoma, use it with caution.
Amitriptyline (Elavil), amoxapine (Asendin), doxepin (Sinequan), imipramine (Tofranil), trimipramine (Surmontil), desipramine (Norpramin), nortriptyline (Pamelor, Aventyl), and protriptyline are examples of tricyclic antidepressants (Vivactil).
Noradrenaline and dopamine reuptake inhibitors (NDRIs)
NDRIs are used to treat depression. NDRIs increase the levels of dopamine and noradrenaline in your brain. NDRIs are also used to help quit smoking and for ADHD.
Examples of NDRIs are bupropion (Zyban).
bupropion for smoking
bupropion for ADHD
Monoamine Oxidase Inhibitors (MAOIs)
Monoamine oxidase inhibitors (MAOIs) are used to treat depression by increasing dopamine, serotonin, tyramine, and norepinephrine levels in your brain.
The FDA has deemed monoamine oxidase inhibitors the second choice to treat it and other mental disorders because of their side effects and safety concerns of the FDA.
Examples of MAOIs are rasagiline (Azilect), selegiline (Eldepryl, Zelapar), isocarboxazid (Marplan), and phenelzine (Nardil), and tranylcypromine (Parnate).
N-methyl D-aspartate (NMDA) antagonists
Antibodies against N-methyl-D-aspartate (NDMA) treat depression by making the brain make more glutamate. A neurotransmitter called glutamate is thought to be involved in depression. NMDA antagonists are only used on people who other antidepressants haven't helped.
One NDMA drug, esketamine (Spravato), has been approved by the FDA to treat depression.
The only way to get esketamine is through a restricted program called Spravato REMS. This is a nasal spray.
After taking medicine, the person may feel tired and disconnected (difficulty with attention, judgment, and thinking). Because of this, esketamine is given in a medical setting where a doctor or nurse can watch for signs of sedation and separation.
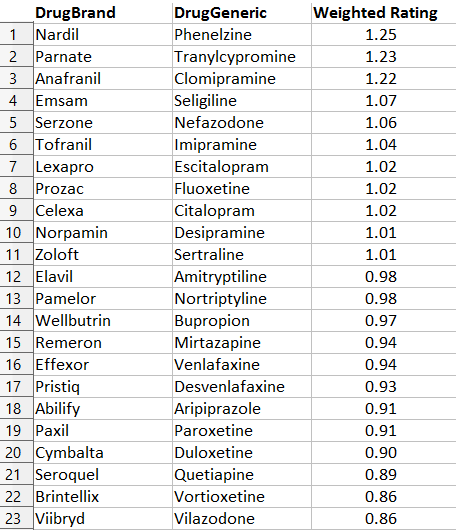
Depression Medication List
Psychotherapy
Psychotherapy can be an excellent way to treat depression because it can help you figure out what might be causing your sad feelings and teach you new ways to deal with them.
Cognitive Therapy (CT)
Cognitive therapy is based on the idea that our thoughts can change how we feel. For instance, if we look for the good in every situation, we are more likely to feel good than if we only think about the bad.
Negative thoughts can cause or make depression worse. When you keep having evil thoughts over and over again, it's hard to feel good. Cognitive therapy helps people learn to recognize negative thought patterns (called cognitive distortions) and change them into more positive ones, which can improve their mood.
Behavioral Therapy (BT)
Cognitive therapy focuses on changing the negative thoughts that lead to depression. On the other hand, behavioral therapy focuses on changing the actions that affect feelings. Behavioral activation is a crucial part of behavioral therapy for depression. This means helping patients do things that will make them feel better about themselves.
Cognitive-Behavioral Therapy (CBT)
Because cognitive therapy and behavioral therapy work well together to treat depression and anxiety disorders, they are often used in cognitive behavioral therapy (CBT). CBT tries to change both the negative ways of thinking and the actions that lead to depression.
Your therapist may ask you to keep a journal to write down what happened during the week and how you felt about it. Automatic adverse reactions are one way of thinking you might work on during CBT. All-or-nothing thinking and overgeneralization are two other types of response patterns. These are both common cognitive distortions.
Once you recognize your response patterns, you and your therapist will work together to learn new ways to think and act. You could also positively talk to yourself.
Depression Test
There isn't a single test for depression; a series of tests are performed to diagnose it. Your doctor diagnoses the depression based on symptoms or physiological evaluation.
In most cases, they may ask a series of questions to test it.
- thoughts
- mood
- apatite
- activity
- sleep schedule
Because depression can be associated with other health issues, your healthcare provider may do a physical exam and prescribe blood testing. It can sometimes be triggered by thyroid issues or a vitamin D shortage.
It is crucial not to disregard depression's signs. If your mood doesn't improve or grows worse, seek medical care. It is a severe mental disorder with the potential for repercussions.
If we left it untreated, it might affect the following conditions,
- Weight gain or weight loss
- physical pain
- Mental disorder
- social isolation
- self-harm
Major depressive disorder
The most severe condition of depression is major depressive disorder (MDD). Depression is defined by emotions of prolonged sadness, hopelessness, and worthlessness that do not resolve by themselves.
To be diagnosed with clinical depression, you must exhibit at least five of the following symptoms for at least two weeks:
- Depressed for the majority of the day
- disinterest in most routine activities
- notable weight loss or increase
- Sleeping excessively or being unable to sleep
- slowed thought or motion
- daily weariness or low energy levels
- sentiments of inadequacy or shame
- Lack of concentration or hesitancy
- repeated thoughts of suicide or death
The American Psychiatric Association refers to the subtypes of major depressive illness as "specificities."
These include the following list,
- peripartum onset, during pregnancy or right after giving birth
- seasonal patterns
- melancholic features
- psychotic features
- catatonia
- atypical features
- anxious distress
- mixed features
- Persistent depressive disorder
- Dysthymia was the last name given to what is now known as persistent depressive disorder (PDD). It's a depression that lasts longer but isn't as severe.
The symptoms must have been present for at least two years to arrive at a diagnosis. Because it lasts for a more extended amount of time than major depression, persistent depressive disorder (PDD) might have a more significant impact on your life.
People who have PDD often have the following behaviors:
- lose interest in regular activities throughout the day
- feel hopeless
- low levels of productivity
- have a humble opinion of oneself
Successful treatment of depression is possible; nevertheless, patients must adhere strictly to their treatment plans.
Depression can make day-to-day life challenging, but getting therapy can help improve your overall quality of life. Discuss the options available with your healthcare provider.
Postpartum Depression
Postpartum depression is a type of depression that can occur after a woman has given birth to a child. It is a prevalent condition that can occur after pregnancy and affects one in every nine new parents.
After giving birth, it is not uncommon for new mothers to experience "baby blues," sometimes as feelings of melancholy or emptiness. These symptoms typically disappear after a couple of days for the majority of people.
However, if your feelings of sadness, hopelessness, or emptiness persist for more than two weeks after giving birth, you may suffer from postpartum depression.
Postpartum depression can present itself with symptoms ranging from moderate to severe and can include the following:
- having no energy or motivation
- eating too little or too much
- sleeping too little or too much
- having trouble focusing
- having memory problems
- feeling restless or moody
- feeling sad, hopeless, or overwhelmed
- having thoughts of hurting the baby or yourself
- not having an interest in the baby, feeling disconnected, or as if your baby is someone else's
It is believed that the significant hormonal shifts that occur after pregnancy cause postpartum depression.
When a person with specific bipolar disorder goes through a depression episode, they are said to be suffering from bipolar depression.
The mental condition known as bipolar disorder is characterized by noticeable shifts in a person's mood, energy level, capacity for concentration, and ability to carry out routine tasks.
There are three subtypes of mental illness known as bipolar disorder. These subtypes include manic episodes, also known as periods in which a person feels notably "up," exhilarated, or energized, and depressive episodes, often known as periods in which a person feels "down," sad, or hopeless.
It may be difficult for someone with bipolar disorder to identify the negative consequences of each "mood episode."
Depression and Anxiety
A person can experience both anxiety and depression at the same time. According to research, approximately seventy percent of patients who suffer from depressive disorders also experience anxiety symptoms.
Depression and anxiety, which are thought to be caused by distinct causes, can produce several symptoms that are pretty similar to one another, including the following:
- irritability
- having trouble remembering things or concentrating can be a challenge.
- sleep troubles
In addition, several therapies for the two disorders can be combined. Treatment options for anxiety and depression include the following: - cognitive behavioral therapy and other types of therapy
- medication
- alternative treatments, such as hypnosis and acupuncture
Make an appointment with your primary care physician if you are concerned that you may be displaying symptoms of one of these disorders, or both, to receive medical advice and treatment. You and they can collaborate to determine the coexisting symptoms of anxiety and depression and the treatments available for those symptoms.
Depression and obsessive-compulsive disorder (OCD)
The anxiety illness is known as obsessive-compulsive disorder (OCD) and falls into the category of anxiety disorders. It induces thoughts, urges, and worries that are not desirable (obsessions).
Compulsions are compulsive activities or rituals that a person feels compelled to carry out repeatedly in the hope that doing so may reduce the stress caused by their obsessions.
People diagnosed with OCD typically find that their obsessions and compulsions repeat themselves in a cycle. If you engage in these actions, you may have the experience of being alone. This can result in you withdrawing from friends and other social situations, which raises the likelihood that you will develop depression.
It is not unheard of for someone who suffers from OCD to struggle with depression. The presence of one anxiety condition can make it more likely that you will also suffer from another. People who suffer from OCD are up to 80% more likely to experience significant depressive episodes.
This dual diagnosis is also a cause for concern for youngsters. They might experience a sense of oddness due to their obsessive activities, which might have originated at a young age. That can result in the youngster isolating themselves from their friends, increasing the likelihood of a child's depression.
Depression in pregnancy
People typically experience a lot of joy during their pregnancies. It is nevertheless not uncommon for a pregnant woman to share feelings of despair.
Symptoms of depression in pregnancy are given below
- persistent sadness
- troubles concentrating or remembering
- sleep problems, including insomnia or sleeping too much
- thoughts of death or suicide
- changes in appetite or eating habits
- feeling hopeless
- anxiety
- losing interest in activities and things you previously enjoyed
Talk therapy and other natural therapies may make up the entirety of the treatment for depression during pregnancy.
It is unknown which antidepressants are the safest for pregnant women to take, despite the fact that some pregnant women take antidepressants. Your healthcare practitioner may suggest you give an alternate treatment a shot until after your child's birth.
Even after the baby is born, there is still a chance of developing postpartum depression. Postpartum depression, also known as a major depressive disorder with a peripartum start, is a severe condition affecting women who have recently given birth.
Data collected from Medical Buck.